| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 5, October 2022, pages 225-231
The Supportive Role of Provocative Maneuvers and Impedance Clearance in Detecting Ineffective Esophageal Motility
Virali Shaha, Alla Turshudzhyanb, Alexandra Mignuccia, Micheal Tadrosa, c
aDivision of Gastroenterology and Hepatology, Department of Medicine, Albany Medical College, Albany, NY, USA
bDepartment of Internal Medicine, University of Connecticut, Farmington, CT, USA
cCorresponding Author: Micheal Tadros, Division of Gastroenterology and Hepatology, Department of Medicine, Albany Medical College, Albany, NY 12309, USA
Manuscript submitted June 27, 2022, accepted August 25, 2022, published online October 19, 2022
Short title: Provocative Maneuvers in Detecting IEM
doi: https://doi.org/10.14740/gr1552
| Abstract | ▴Top |
Background: Ineffective esophageal motility (IEM) is one of the most common esophageal motility disorders. However, the definition of IEM has evolved. Chicago classification version 4.0 (CCv4.0) made IEM parameters more stringent with greater than 70% of ineffective wet swallows (WS) necessary to diagnose conclusive IEM. Of the ineffective swallows, 50-70% are deemed “inconclusive cases”. This study sought to determine whether provocative maneuvers, including multiple rapid swallows (MRS) and apple viscous swallows (AVS), and impedance clearance can provide supportive information for inconclusive IEM disorders based on CCv4.0.
Methods: Esophageal motility data on 100 patients were analyzed. All patients completed WS and at least one additional swallow test (MRS and/or AVS). Patients were classified as having conclusive IEM, inconclusive IEM, or normal motility. IEM features detected on MRS/AVS and incomplete bolus clearance were recorded. Percentage of agreement between IEM features and incomplete bolus clearance was calculated for each motility group.
Results: Ten patients had conclusive IEM, nine had inconclusive IEM, and 32 had normal motility. There was 70% agreement between IEM features and incomplete bolus clearance with conclusive IEM, 33% agreement with inconclusive IEM, and 9% agreement with normal motility. There was significantly more agreement in the conclusive and inconclusive IEM groups than in the normal motility group (P = 0.0003).
Conclusions: Combinational follow-up testing with provocative maneuvers and impedance clearance may assist with risk stratification of IEM patients and assist in further management of inconclusive IEM. MRS and AVS can detect unique IEM features that may help with preoperative management of inconclusive IEM.
Keywords: Ineffective esophageal motility; Chicago classification; Manometry; Esophagus; Impedance clearance
| Introduction | ▴Top |
Over the past decade, ineffective esophageal motility (IEM) has significantly increased in prevalence becoming one of the most common esophageal motility disorders [1, 2]. Presenting symptoms of IEM can overlap with those of gastroesophageal reflux disease (GERD), which poses a diagnostic challenge for physicians evaluating patients with IEM disorders [3, 4]. As a result, IEM is frequently over-diagnosed [5]. Establishing correct diagnosis becomes especially important for patients undergoing foregut surgery as it can determine surgical outcomes. Laparoscopic Nissen fundoplication (LNF) remains the surgical treatment of choice for patients with GERD. However, if it is performed in patients with underlying motility disorder, dysphagia may worsen post-fundoplication [6, 7].
The definition of IEM has evolved over the years with introduction of new diagnostic methods. While the initial definition involved small and large defects in peristalsis, the Chicago classifications v3.0 (2015) defined ineffective swallows as a distal contractile integral (DCI) of less than 450 mm Hg s cm with greater than 50% ineffective swallows [8]. This helped eliminate the difference between weak and failed swallows but resulted in overdiagnosis of IEM [8]. The most recent Chicago classification v4.0 (CCv4.0) (2021) imposed more stringent criteria defining IEM as greater than 70% ineffective swallows or greater than 50% failed peristalsis, which improved diagnostic precision, but resulted in cases with 50-70% of ineffective swallows considered inconclusive IEM [9]. As a result, CCv4.0 recommends follow-up supportive testing for these patients [9]. The process of confirming IEM cases with provocative maneuvers remains non-standardized across clinical practice. Past studies demonstrated evidence that multiple rapid swallows (MRS) and impedance clearance may help confirm IEM [9]. Our study aimed to expand on the current literature and further explore ways provocative maneuvers can assist physicians in diagnosing inconclusive cases of IEM.
MRS is a provocative maneuver that may detect abnormal contractions and peristaltic reserve otherwise missed on high-resolution manometry (HRM) [10]. Min et al (2015) showed that abnormal contractions on MRS with DCI less than 450 mm Hg s cm were correlated with greater risks for prolonged bolus clearance and poor bolus transit [10]. Additionally, Price et al (2015) further supported that MRS can detect patterns of abnormal pathophysiology that were not identified on HRM [11]. Aside from peristaltic reserve, percentage of failed swallows, viscous swallow-induced dysphagia, and impendence clearance are other useful measures for patients with inconclusive IEM [12, 13]. Previous literature suggests that impaired bolus clearance with ≥ 30% failed contractions was a sensitive and specific indicator for IEM [14, 15].
The goal for our study was to investigate whether MRS, apple viscous swallows (AVS), and impedance clearance could be used as supportive testing for confirmed, minor, or inconclusive cases of IEM.
| Materials and Methods | ▴Top |
Subjects and study protocol
This was a retrospective study of 100 patients with a known esophageal dysfunction at a tertiary academic gastroenterology clinic in Albany, NY. Patients included in this study underwent HRM evaluation from July 1, 2017 to March 1, 2020. Institutional Review Boards exemption was obtained prior to starting the study. The study was conducted in compliance with the ethical standards of the responsible institution.
Inclusion criteria included any patient above the age of 18, presenting with an esophageal indication, and completed both follow-up swallow tests (MRS and AVS). Exclusion criteria included any patient under the age of 18, did not complete any swallow tests, or had high risk of aspiration. Patients had a variety of indicators for esophageal assessment including reflux symptoms, dysphagia, chest pain, and preoperative preparedness. Fourteen patients were excluded due to incomplete provocative swallow evaluations or suspected achalasia with high risk for aspiration. Of the original 100 patients, 70 patients were able to undergo all the swallow tests (wet swallow (WS), AVS, and MRS). Demographic information was collected and outlined for these 70 patients (Table 1). The 70 patients were then categorized by motility patterns based on CCv4.0 criteria. ManoView ESO 3.3 software (Medtronic Inc., Shoreview, MN, USA) was utilized to evaluate MRS, AVS, and WS data (Figs. 1 and 2).
 Click to view | Table 1. Demographic Breakdown by Age, Gender, and Body Mass Index (n = 70) |
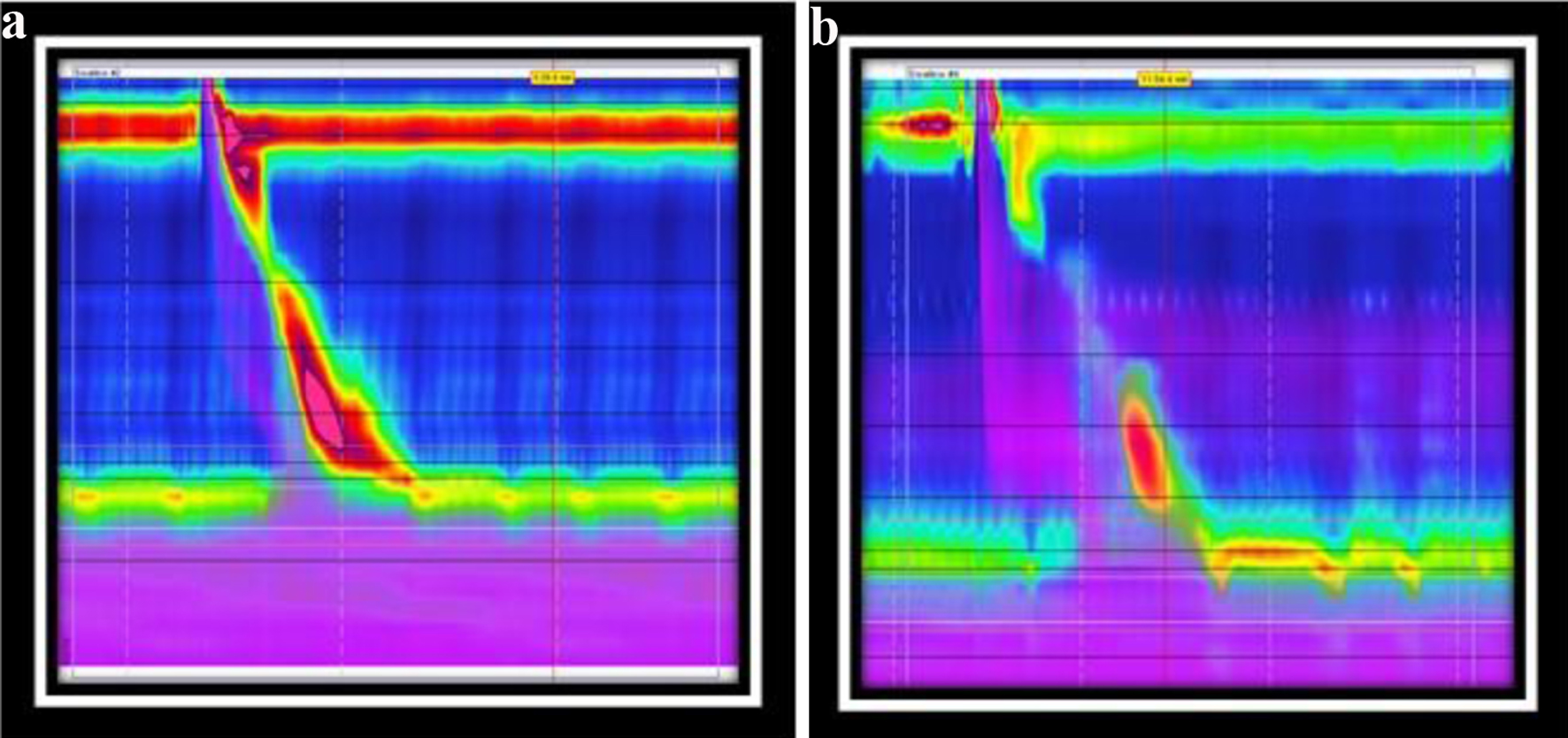 Click for large image | Figure 1. (a) Normal contraction and complete impedance clearance on wet swallow. (b) Weak peristaltic contractions with incomplete impedance clearance on wet swallow. |
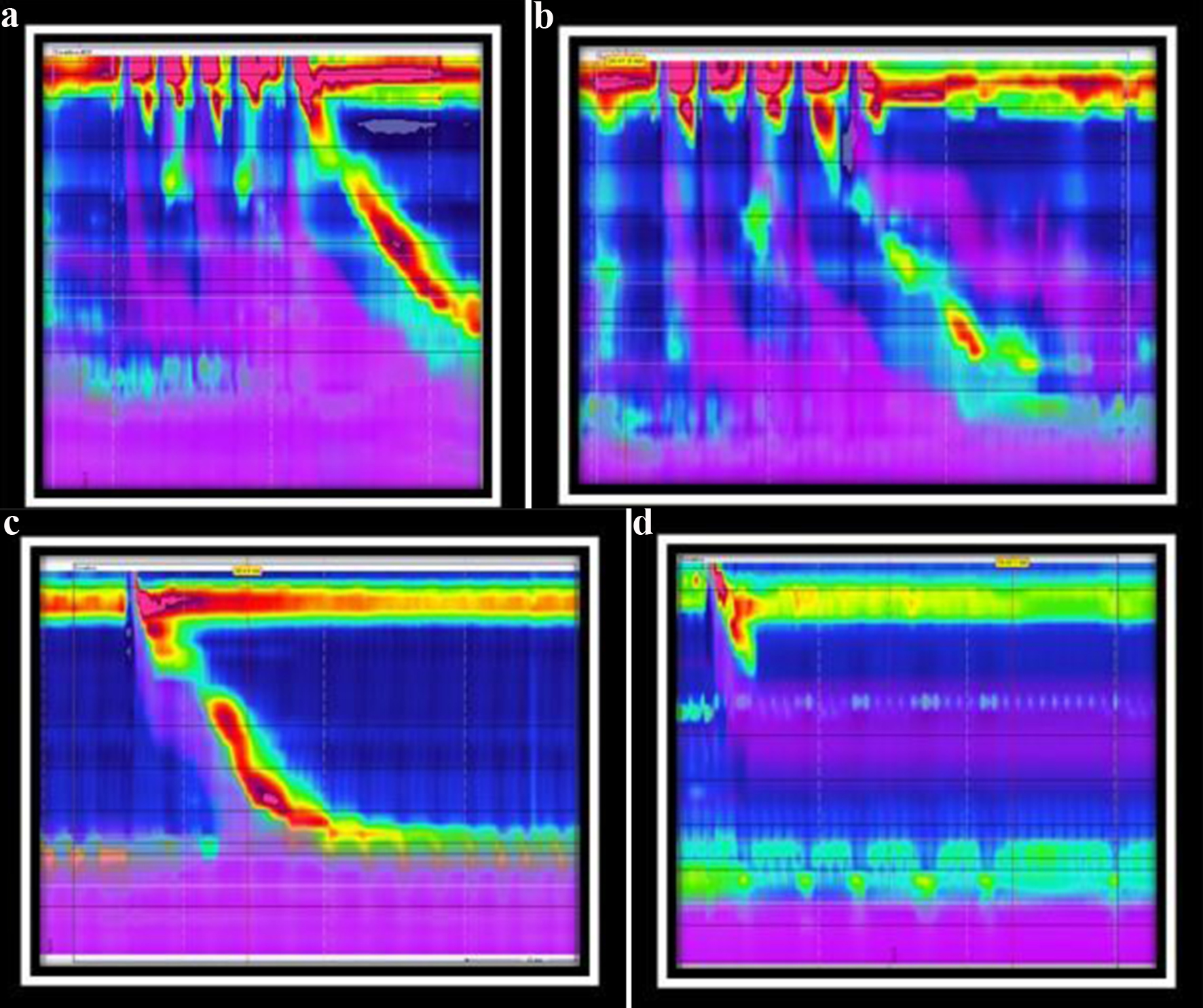 Click for large image | Figure 2. (a) Normal contraction on MRS swallow. (b) IEM features from MRS swallow. (c) Normal contraction and complete impedance clearance on AVS swallow. (d) IEM features and incomplete impedance clearance from a failed AVS swallow. IEM: ineffective esophageal motility; MRS: multiple rapid swallows; AVS: apple viscous swallows. |
Parameters collected
CCv4.0 was used to evaluate each patient’s esophageal motility. Based on recent CCv4.0 definitions, patients were classified as either conclusive IEM, inconclusive IEM, or normal.
For each patient, the following measures were collected: 1) incomplete bolus clearance; 2) IEM features from MRS; 3) IEM features from AVS; 4) absent peristalsis from MRS; and 5) absent peristalsis from AVS.
Definitions
Incomplete bolus clearance was defined as incomplete impedance clearance in ≥ 20% for WS, ≥ 30% for AVS [14]. IEM features from MRS results were defined as weak peristaltic reserve (DCI ratio < 0.85) or absent peristalsis [16]. IEM features from AVS results were defined as > 50% of ineffective contractions or absent peristalsis [17]. Absent peristalsis was defined as 100% failed swallows.
Statistical analysis
Analysis of variance (ANOVA) tests were conducted to determine statistical significance. A dedicated computerized software package known as GraphPad Prism was utilized to carry out these tests. P values less than 0.05 were considered statistically significant.
| Results | ▴Top |
Among the 70 patients, 10 patients had conclusive IEM, nine patients had inconclusive IEM, and 32 patients had normal motility based on CCv4.0. The remaining patients were excluded from further analysis because they had different motility patterns, including 16 patients with esophagogastric outflow obstruction (EGJOO), one with distal esophageal spasm, and two with absent contractility. For the included 51 patients, IEM features detected from MRS and AVS were also overlapped with incomplete impedance clearance from AVS and WS to highlight patterns and discrepancies (Tables 2, 3, Figs. 1, 3).
 Click to view | Table 2. Breakdown of Patients by Motility Diagnosis for IEM Features and Incomplete Bolus Clearance Detected on Each Swallow Test |
 Click to view | Table 3. Breakdown of Patients With Overlapped Results of IEM Features and Bolus Clearance |
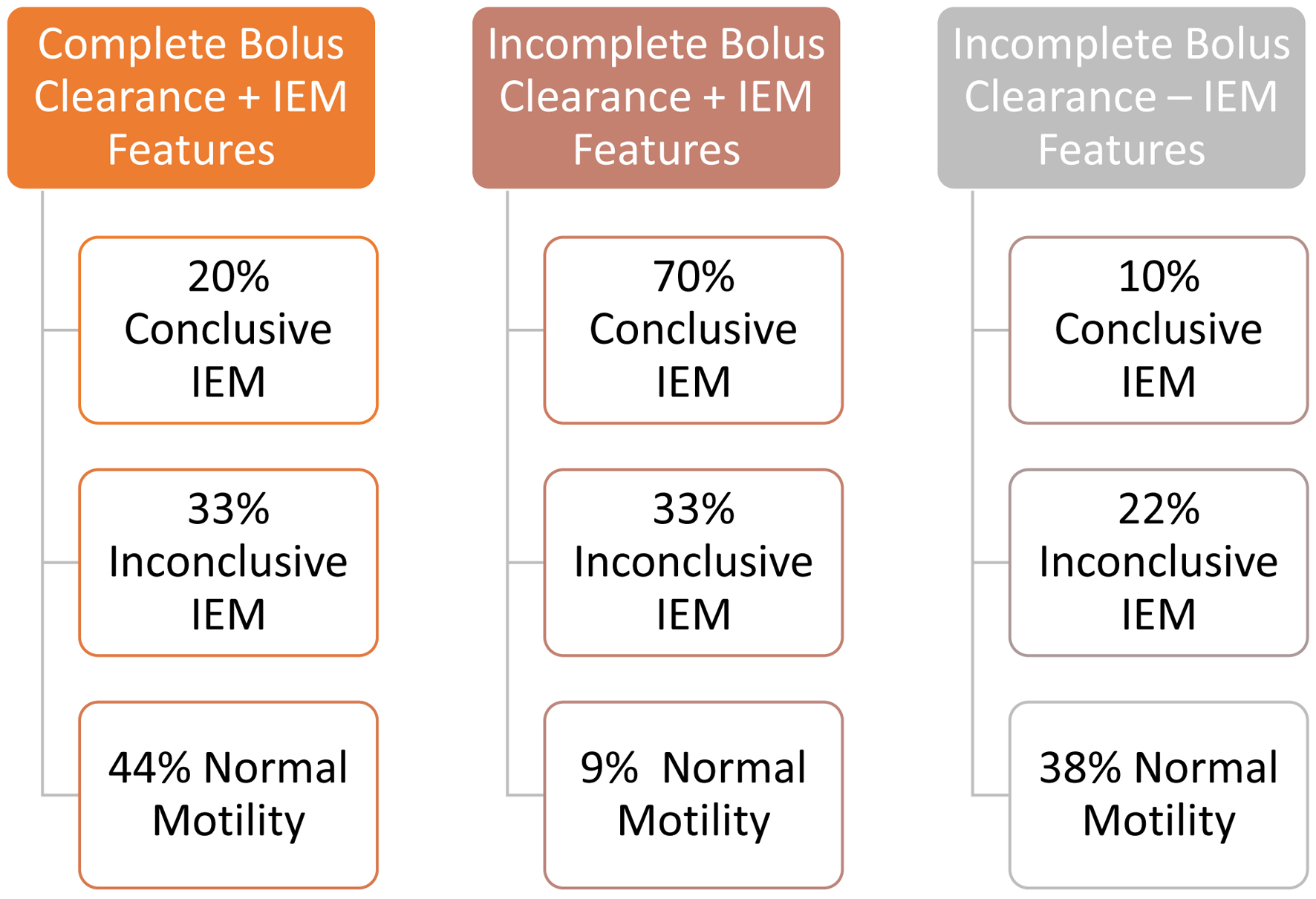 Click for large image | Figure 3. Percentage of patients with overlap of IEM features and incomplete bolus clearance based on their motility status. IEM: ineffective esophageal motility. |
Among the 10 patients with conclusive IEM based on CCv4.0, seven (70%) patients had both IEM features on MRS/AVS and incomplete bolus clearance, two (20%) patients had IEM features on MRS/AVS with complete bolus clearance, and one (10%) patient had no IEM features on MRS/AVS but had incomplete bolus clearance (Table 2, Fig. 2). In patients with conclusive IEM, there was a 70% agreement between IEM swallow features and incomplete bolus clearance results (Fig. 4).
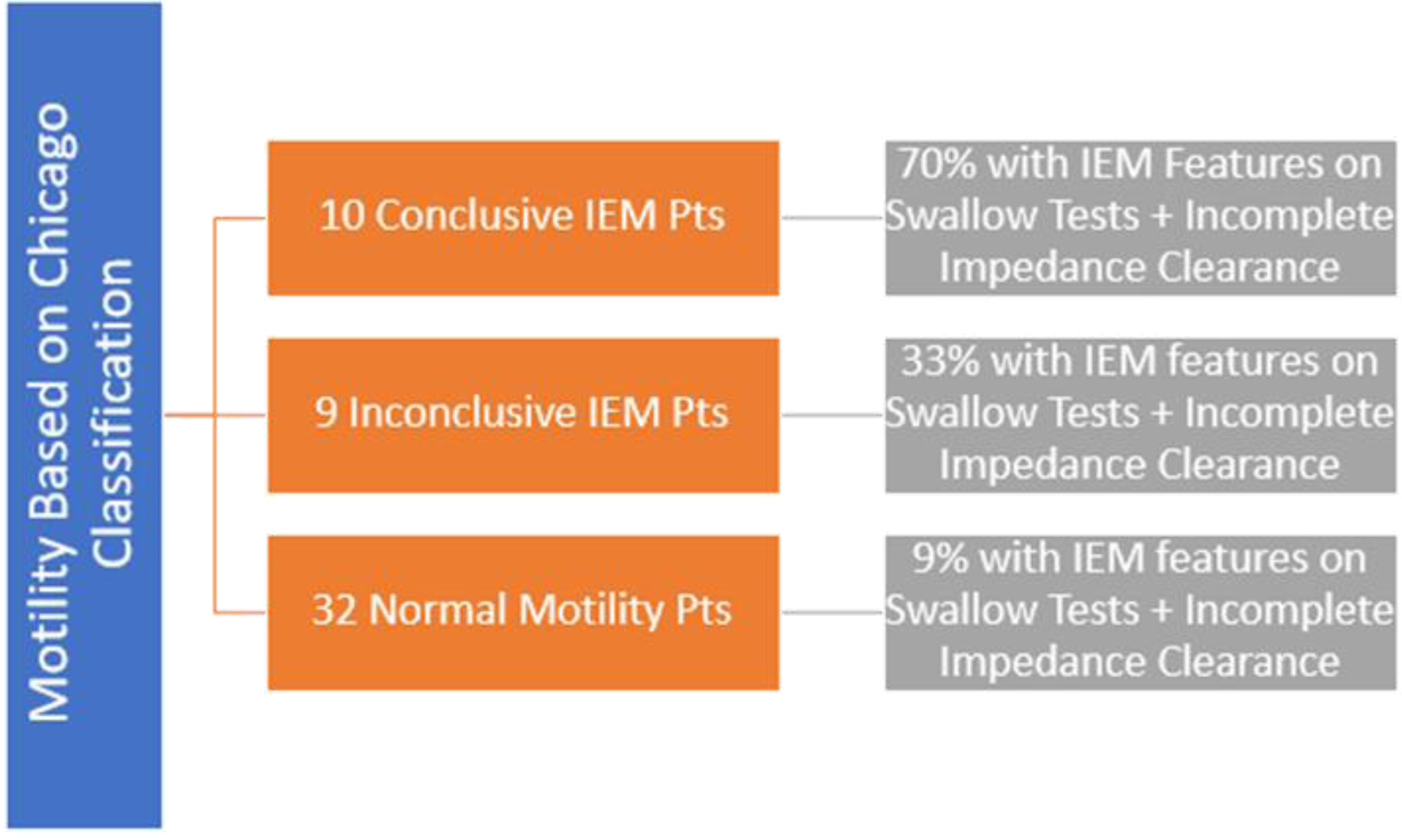 Click for large image | Figure 4. Agreement rates between IEM features and impedance clearance for conclusive IEM, inconclusive IEM, and normal motility patients. IEM: ineffective esophageal motility. |
Among the nine patients with inconclusive IEM based on CCv4.0, three (33%) patients had both IEM features on MRS/AVS and incomplete bolus clearance, three (33%) patients had IEM features on MRS/AVS with complete bolus clearance, and two (22%) patients had no IEM features on MRS/AVS but had incomplete bolus clearance (Table 2, Fig. 2). In patients with inconclusive IEM, there was a 33% agreement between IEM swallow features and incomplete bolus clearance results (Fig. 4).
Among the 32 patients with normal motility based on CCv4.0, three (9%) patients had both IEM features on MRS/AVS and incomplete bolus clearance, 14 (44%) patients had IEM features on MRS/AVS with complete bolus clearance, and 12 (38%) patients had no IEM features on MRS/AVS but had incomplete bolus clearance (Table 2, Fig. 2). For patients with normal motility, there was a 9% agreement between IEM swallow features and incomplete bolus clearance results (Fig. 4).
There was significantly more agreement between IEM features detected by swallow maneuvers and impedance testing in the conclusive IEM group and inconclusive IEM group than in the group with presumed normal motility per CCv4.0 (70% vs. 33% vs. 9%; P = 0.0003). However, the conclusive IEM group did have significantly more agreement among its follow-up testing than the inconclusive IEM group (P = 0.001).
A subset analysis was conducted to compare IEM features detected by MRS and AVS. Among the 70 patients who completed both MRS and AVS, 13 patients had IEM features detected on MRS (two patients with absent peristalsis), 17 patients had IEM features detected on AVS (four patients with absent peristalsis), and 10 patients had IEM features detected on both MRS and AVS (two patients with absent peristalsis). Four patients had absent peristalsis with only AVS, whereas two patients had absent peristalsis with only MRS. Among the four patients who only failed AVS, one patient was in the conclusive IEM group and three patients were in the inconclusive IEM group (Table 2). Follow-up AVS testing was particularly beneficial for the three patients in the inconclusive IEM group because these patients had severe hypokinetic disorders that missed detection via MRS.
| Discussion | ▴Top |
Our study confirmed that supportive testing with provocative maneuvers and impedance clearance provides physicians with valuable insight into confirmed, minor, and unclear cases of IEM. The combination of swallow testing with MRS and AVS in conjunction with impedance clearance provides additional insight into a patient’s esophageal motility.
The addition of swallow maneuvers and impedance clearance confirmed the findings based on CCv4.0 for patients with conclusive IEM. The data gathered from provocative maneuvers indicated that IEM is a spectrum, with some patients having more severe features than others. Seventy percent of conclusive IEM patients had IEM features detected on AVS/MRS and incomplete impedance clearance. Interestingly, these patients also had more severe forms of IEM when compared with the rest of patients, based on symptomatic presentation and high-resolution manometric measurements. These added findings may assist physicians and surgeons in deciding treatment options for IEM based on risk stratification.
The supportive testing with provocative maneuvers and impedance clearance was particularly advantageous for patients with inconclusive IEM based on CCv4.0 guidelines. At least one IEM feature and/or incomplete impedance clearance was found in 89% of patients with inconclusive IEM. AVS and impedance clearance identified features of IEM in 33% of patients and detected no features of IEM in 11% of patients. This tailored proper medical management, such as determining preoperative preparedness. It is traditionally recommended by Chicago classification guidelines to follow-up IEM diagnosis with MRS to determine peristaltic reserve [9]. However, in this study, AVS was also beneficial in highlighting features of IEM that were missed by MRS. For example, AVS uniquely identified severe hypokinesis in three patients with inconclusive IEM based on CCv4.0. AVS detected unique IEM features in 24% of patients that were missed by MRS, and MRS detected unique IEM features in 19% of patients that were missed by AVS. Each swallow test has an individual way of eliciting IEM features; therefore, combinational supportive testing could be considered in the preoperative setting. Furthermore, impedance clearance testing was diagnostically important in stratifying high-risk patients and providing concordance with swallow test results.
For patients with normal motility based on CCv4.0, supportive testing was helpful in confirming normal motility and highlighting minor IEM features. Ninety percent of patients with normal motility had at least one IEM feature or incomplete bolus clearance detected on supportive testing. While these patients were still classified as normal, it is important to know when patients may have underlying IEM features that could worsen over time. Preventative measures with symptomatic management, nutritional education, and review of medication side effects are critical in preserving normal motility for these patients [5].
Strengths
This is the first study to explore the role of combinational swallow and impedance testing in cases of inconclusive IEM based on CCv4.0. The findings of this study may assist clinicians with follow-up decision making who use Chicago classifications guidelines to diagnose IEM. In addition, this study provides unique insight into IEM features found in patients with conclusive IEM and normal motility that may guide preoperative management.
Weaknesses
Some of the limitations of our study include that the study was retrospective and conducted at a single academic center. The patient size was limited to 100 patients. A larger prospective randomized controlled study should be done to further investigate the utility of impedance clearance and provocative testing.
Conclusion
Currently, Chicago classification guidelines and peristaltic reserve estimated from MRS DCI index provide an excellent framework for patients with severe IEM disorders, but there is little research on cases that are inconclusive. Combinational technology with provocative maneuvers and impedance testing can provide physicians with additional insight into a patient’s esophageal motility. IEM features can further tailor medical and surgical management for patients, stratifying patients from low to high risk. Our study found utility in AVS through detection of severe hypokinesis that was missed by MRS, an important finding for assessing preoperative preparedness. The growing value of impedance clearance in the literature is also supported by our study. We recommend comprehensive follow-up testing with impedance clearance and viscous swallows in conjunction with MRS when evaluating diagnostically challenging cases of IEM.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
There is no conflict of interest to disclose from any of the authors. Dr. Michael Tadros, MD is the guarantor for this article and accepts full responsibility for the conduct of the study.
Informed Consent
Appropriate consent was obtained.
Author Contributions
Virali Shah contributed to study concept, study planning, institutional approval, data collection and analysis, manuscript preparation, edits, and critical review. Alla Turshudzhyan contributed to manuscript preparation, edits, and critical review. Alexandra Mignucci contributed to data collection and analysis, and manuscript preparation. Micheal Tadros contributed to study concept, institutional approval, data collection and analysis, and critical review of manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Alani M, Al-Jashaami L, Mills M, Guha Sushovan, Ratuapli SK. prevalence of esophageal motility disorders in an open access hybrid "Academic - Community Setting" patient population. American Journal of Gastroenterology. 2018;113:S180-S181.
doi - Boland K, Abdul-Hussein M, Tutuian R, Castell DO. Characteristics of consecutive esophageal motility diagnoses after a decade of change. J Clin Gastroenterol. 2016;50(4):301-306.
doi pubmed - Fouad YM, Katz PO, Hatlebakk JG, Castell DO. Ineffective esophageal motility: the most common motility abnormality in patients with GERD-associated respiratory symptoms. Am J Gastroenterol. 1999;94(6):1464-1467.
doi pubmed - Martinucci I, de Bortoli N, Giacchino M, Bodini G, Marabotto E, Marchi S, Savarino V, et al. Esophageal motility abnormalities in gastroesophageal reflux disease. World J Gastrointest Pharmacol Ther. 2014;5(2):86-96.
doi pubmed - Jandee S, Geeraerts A, Geysen H, Rommel N, Tack J, Vanuytsel T. Management of Ineffective Esophageal Hypomotility. Front Pharmacol. 2021;12:638915.
doi pubmed - Kim HJ, Sharma VK, Harold K, Schlinkert R, Crowell MD. Ineffective or "Insignificant" esophageal motility disorder in gastroesophageal reflux disease (GERD). American Journal of Gastroenterology. 2005;100:S32.
doi - Xiao Y, Kahrilas PJ, Kwasny MJ, Roman S, Lin Z, Nicodeme F, Lu C, et al. High-resolution manometry correlates of ineffective esophageal motility. Am J Gastroenterol. 2012;107(11):1647-1654.
doi pubmed - Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-174.
doi pubmed - Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33(1):e14058.
- Min YW, Shin I, Son HJ, Rhee PL. Multiple rapid swallow maneuver enhances the clinical utility of high-resolution manometry in patients showing ineffective esophageal motility. Medicine (Baltimore). 2015;94(40):e1669.
doi pubmed - Price LH, Li Y, Patel A, Gyawali CP. Reproducibility patterns of multiple rapid swallows during high resolution esophageal manometry provide insights into esophageal pathophysiology. Neurogastroenterol Motil. 2014;26(5):646-653.
doi pubmed - Jain A, Baker JR, Chen JW. In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil. 2018;30(6):e13297.
doi pubmed - Meshkinpour H, Eckerling G. Unexplained dysphagia: viscous swallow-induced esophageal dysmotility. Dysphagia. 1996;11(2):125-128.
doi pubmed - Zerbib F, Marin I, Cisternas D, Abrahao L, Jr., Hani A, Leguizamo AM, Remes-Troche JM, et al. Ineffective esophageal motility and bolus clearance. A study with combined high-resolution manometry and impedance in asymptomatic controls and patients. Neurogastroenterol Motil. 2020;32(9):e13876.
doi pubmed - Chugh P, Collazo T, Dworkin B, Jodorkovsky D. Ineffective Esophageal Motility Is Associated with Impaired Bolus Clearance but Does Not Correlate with Severity of Dysphagia. Dig Dis Sci. 2019;64(3):811-814.
doi pubmed - Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108(11):1706-1712.
doi pubmed - Blonski W, Vela M, Safder A, Hila A, Castell DO. Revised criterion for diagnosis of ineffective esophageal motility is associated with more frequent dysphagia and greater bolus transit abnormalities. Am J Gastroenterol. 2008;103(3):699-704.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


