| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 13, Number 6, December 2020, pages 253-259
Cirrhosis Is Associated With Worse Outcomes in Ischemic Colitis: A Nationwide Retrospective Study
Eric Thena, Caitlin Lundb, Dustin J. Uhlenhoppc, e, Tagore Sunkarad, Vinaya Gaduputid
aDivision of Gastroenterology and Hepatology, The Brooklyn Hospital Center - Clinical Affiliate of The Mount Sinai Hospital, Brooklyn, NY, USA
bDepartment of General Surgery, MercyOne Des Moines Medical Center, Des Moines, IA, USA
cDepartment of Internal Medicine, MercyOne Des Moines Medical Center, Des Moines, IA, USA
dDepartment of Gastroenterology and Hepatology, MercyOne Des Moines Medical Center, Des Moines, IA, USA
eCorresponding Author: Dustin Uhlenhopp, MercyOne Des Moines Medical Center, 1111 6th Avenue, Des Moines, IA 50314, USA
Manuscript submitted October 26, 2020, accepted December 17, 2020, published online December 23, 2020
Short title: Cirrhosis Worsens Ischemic Colitis Outcomes
doi: https://doi.org/10.14740/gr1339
| Abstract | ▴Top |
Background: Ischemic colitis (IC) occurs when the blood supply of the large intestine becomes compromised. Cirrhosis is a disease entity in which there is a delicate balance between pro-coagulant and anti-coagulant states. Our aim was to examine the impact cirrhosis has on outcomes in patients with ischemic colitis.
Methods: A retrospective analysis of patients hospitalized with IC in 2017 was evaluated using the National Inpatient Sample database. Baseline demographic data, length of hospital stay (LOS), total hospital charge, rates of colectomy and in-hospital mortality were extracted from the database. Categorical variables were compared using the Chi-square test and continuous variables were compared using t-test.
Results: A total of 29,035 patients with IC were identified, while 420 of these patients also had cirrhosis. Patients with IC and cirrhosis were noted to be younger age at presentation when compared to patients with IC and no cirrhosis (mean 63.9 years vs. 70.4 years; P < 0.001). When comparing both groups, IC patients with cirrhosis were more likely to be male (50% vs. 26.1%; P < 0.001), Black (10.9% vs. 7.6%; P = 0.013) and Hispanic (18% vs. 6.1%; P < 0.001). We found that IC patients with cirrhosis had a longer LOS (7.3 days vs. 4.8 days; P < 0.001), higher total hospital charge ($84,769 vs. $48,347; P < 0.001) and higher mortality rate (10.7% vs. 3.6%; P < 0.001); however, the presence of cirrhosis was not associated with increased odds of undergoing colectomy (odds ratio: 0.31; 95% confidence interval: 0.07 - 1.27; P = 0.104).
Conclusions: The presence of cirrhosis is associated with increased odds of in-hospital mortality in those presenting with IC. This compounds the already high rates of mortality in patients that undergo surgery for IC and could reflect lack of reserve to withstand the ischemic episode in the setting of cirrhosis. Though odds of undergoing colectomy is not increased, patients with cirrhosis warrant closer observation.
Keywords: Ischemic colitis; Cirrhosis; Mortality; Colectomy; National Inpatient Sample
| Introduction | ▴Top |
Ischemic colitis (IC) is a gastrointestinal (GI) disorder that occurs when the blood supply of the large intestine becomes compromised and is often categorized in occlusive versus non-occlusive causes. Cirrhosis is a disease entity in which there is a delicate balance between pro-coagulant and anti-coagulant states. If altered, this may result in excessive bleeding or clot formation.
It is known that portal hypertension leads to associated colopathies, most notably colonic vascular ectasias and rectal varices [1]. Dilated and congested capillaries, and capillaries with irregularly thickened walls are seen in higher numbers in patients with portal hypertension [2]. It has been noted that colonic wall changes can be seen on computed tomography (CT) scans in higher rates in patients with cirrhosis, with up to 37% having colonic wall thickening notable on CT [2].
Classic IC usually affects the left side of the colon most commonly in “watershed areas” such as hepatic flexure and sigmoid colon [3]. The normal colonic response to ischemia is vasodilation; however, in patients with portal hypertension, there is little reserve to meet the demand of ischemia. Cirrhosis and associated portal venous hypertension result in microvascular colopathies, which can lead to venous congestion and may make the colon more susceptible to ischemic insults [4]. While colopathies associated with portal hypertension are more commonly seen in the right hemi-colon, it can be assumed that the colon would be more susceptible to ischemic insult due to the lack of compensatory mechanisms [4].
Although uncommon, lower GI bleeding in cirrhotic patients is associated with a high mortality rate of 17% [5]. Ischemic bowel disease accounts for 3-9% of all cases of LGIB and increases with advancing age. This would be expected to be higher in patients with cirrhosis or predisposing factors for ischemia [5].
Our study aimed to examine the impact cirrhosis has on the severity of IC. The specific study objectives were to characterize if there was a significant difference in hospital length of stay (LOS) between patients with IC alone as compared to those with IC and cirrhosis. We also evaluated if there was a difference in rate of in-hospital colectomy for the two groups.
| Materials and Methods | ▴Top |
Data source
This was a retrospective cohort study of patients admitted to acute care hospitals in the United States of America (US) with IC in the year 2017. Patients were extracted from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) database. The NIS is the largest publicly available inpatient database in the USA and is sponsored by the Agency for Healthcare Research Quality (AHRQ). The 2017 NIS sampling frame includes data from 46 states, covering more than 97% of the total US population [6]. A 20% probability sample was collected and subsequently weighted to ensure that the selected population was nationally representative. Each admission in the database was assigned one principal diagnosis, up to 39 secondary diagnoses, and up to 25 procedures. These variables are defined via International Classification of Disease, 10th revision, and Clinical Modification (ICD-10-CM) codes.
Study population
Patients with the principal ICD-10-CM diagnosis of IC were included in our study. After extracting these patients, they were then divided into two groups. The first group consisted of patients with IC as the principal diagnosis who did not have cirrhosis listed as a secondary diagnosis. The second group consisted of patients with IC as the principal diagnosis while concurrently having the secondary diagnosis of cirrhosis from any cause.
Study variables
We extracted baseline patient and hospital characteristics for each admission that met our inclusion criteria. Patient characteristics included age (years), gender, race (White, Black, Hispanic, Asian or Pacific Islander, Native American), insurance type and Charlson comorbidity index. Hospital characteristics included hospital region and hospital bed size. Additionally, we extracted the total number of colectomies (via ICD-10-CM procedure codes) that were performed for each individual admission across all study groups. Other variables that were extracted included total number of deaths, LOS and total hospital charge. Total hospital charge refers to the amount of money each hospital billed the payer for the service provided during each admission.
Outcomes
Our primary endpoint was to elucidate if there was a statistically significant difference in LOS between patients with IC alone compared to those with IC and cirrhosis. Secondary endpoints included comparing the proportions of colectomies performed, total hospital charges and total deaths between the two groups.
Statistical analysis
Statistical analysis was conducted using STATA software, version 15.0 (StataCorp., College Station, Texas, USA). NIS provides discharge level weights that facilitate estimating the total number of patients with IC across the USA. Descriptive statistics were used to describe the characteristics of the cohorts of patients with IC alone, and those with IC and cirrhosis. Fisher’s exact test was used to compare proportions, and Welch’s t-test was used to compare means between the cohorts. Multivariant logistic regression analyses were conducted to evaluate factors that were associated with in-hospital colectomy and in-hospital mortality. Variables with a P-value ≤ 0.1 on univariant analysis were entered and further computed on the multivariate logistic regression model. Associations between the study and outcome variables were described using odds ratio (OR) at 95% confidence interval (CI). A two-tailed P-value < 0.05 was considered statistically significant.
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Institutional Review Board approval is not required for this study.
| Results | ▴Top |
Patient and hospital characteristics
Figure 1 shows a flow diagram for the patients included in our study. A total of 29,035 patients with IC were identified. Of those, a total of 28,615 patients had IC with no cirrhosis, and 420 patients had IC with concurrent cirrhosis. Patients with IC and cirrhosis were found to have a statistically significant younger age of presentation when compared to patients with IC and no cirrhosis (mean 63.9 years vs. 70.4 years; P < 0.001). When compared to patients without cirrhosis, IC patients with cirrhosis were more likely to be male (50% vs. 26.1%; P < 0.001), Black (10.9% vs. 7.6%; P < 0.013) and Hispanic (18% vs. 6.1%; P < 0.001). It is important to note however, most patients were predominately White in both groups (Table 1). Similarly, there were statistically significant differences in hospital region, hospital bed size and insurance between the two groups (Table 1).
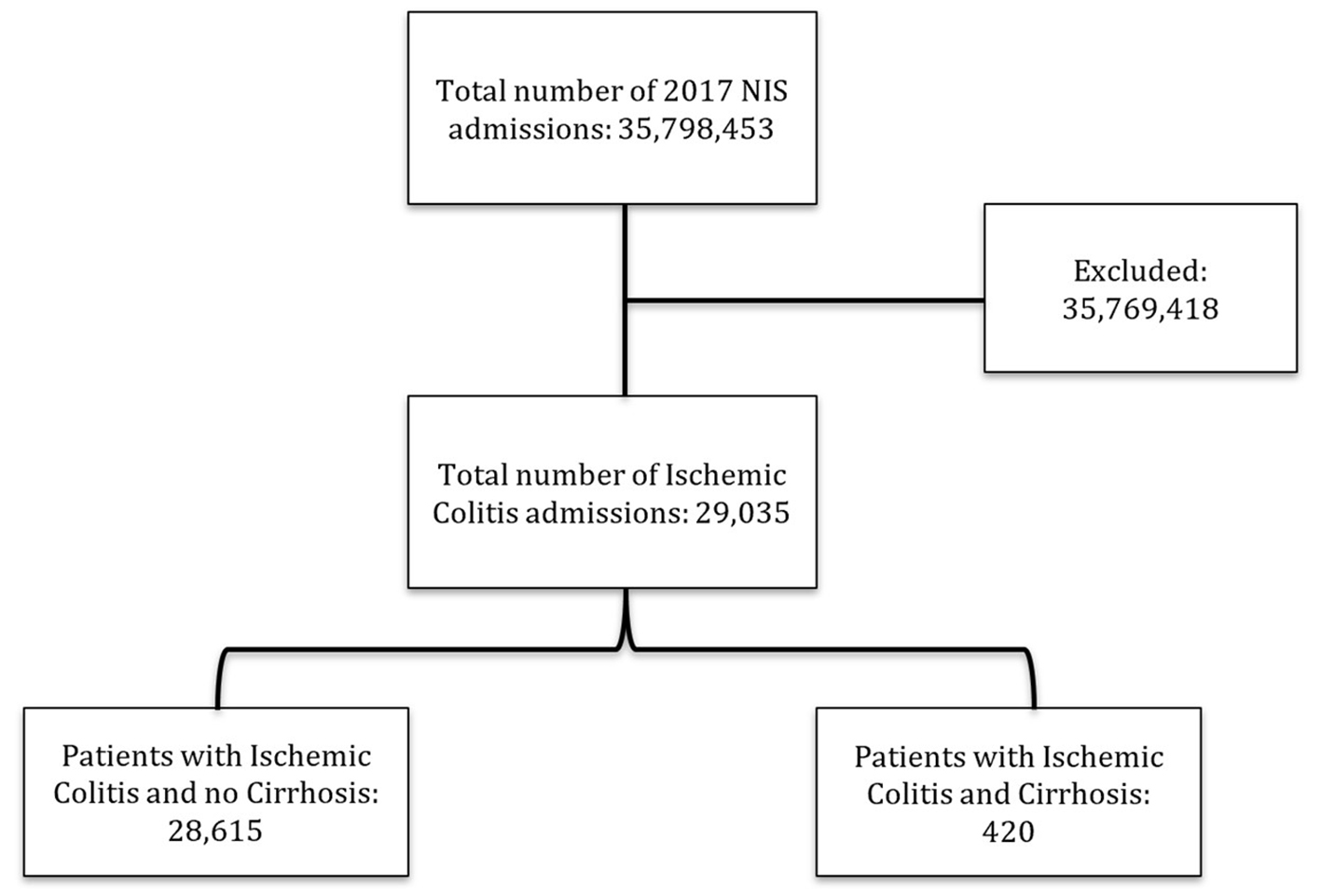 Click for large image | Figure 1. Flow diagram of patient selection. |
 Click to view | Table 1. Baseline Demographic Characteristics |
In-hospital colectomy rates
When comparing rates of in-hospital colectomies, patients with IC and cirrhosis had a statistically significant decreased rate of colectomy when compared with patients with IC without the secondary diagnosis of cirrhosis (2.3% vs. 5.1%; P = 0.015) (Table 2). However, these findings were not reflected on multivariate analysis (Table 3). When adjusting for age, gender, race and co-morbid conditions (atrial fibrillation, coronary artery disease, congestive heart failure, peripheral vascular disease, end-stage renal disease, hypertension and diabetes mellitus), the presence of cirrhosis was not associated with a statistically significant difference in odds of undergoing colectomy (OR: 0.31; 95% CI: 0.07 - 1.27; P = 0.104). Atrial fibrillation was associated with statistically significant increased odds of in-hospital colectomy (OR: 1.95; 95% CI: 1.42 - 2.64; P < 0.001). Patients who were Black or Hispanic were also at increased odds of colectomy (OR: 1.68; 95% CI: 1.11 - 2.53; P = 0.013 and OR: 6.24; 95% CI: 1.83 - 21.30; P = 0.003, respectively).
 Click to view | Table 2. Hospital Outcomes |
 Click to view | Table 3. Multivariate Analysis for In-Hospital Colectomy |
Resource utilization and mortality
The mean LOS, total hospital charges and total deaths for both groups are presented in Table 2. Patients with IC and cirrhosis had statistically significant higher total hospital charge ($84,769 vs. $48,347; P < 0.001) and longer LOS (7.3 days vs. 4.8 days; P < 0.001). Regarding in-hospital mortality rates, patients with IC and cirrhosis had a statistically significant increased mortality rate when compared to patients without cirrhosis (10.7% vs. 3.6%; P < 0.001). These findings were sustained on multivariate analysis (Table 4). When adjusting for age, gender, race and co-morbid conditions (atrial fibrillation, coronary artery disease, congestive heart failure, peripheral vascular disease, end-stage renal disease, hypertension and diabetes mellitus), the presence of cirrhosis was associated with statistically significant increased odds of in-hospital mortality (OR: 3.15; 95% CI: 1.46 - 6.79; P = 0.003). Multivariate analysis demonstrated that atrial fibrillation (OR: 2.31; 95% CI: 1.68 - 3.16; P < 0.001), peripheral vascular disease (OR: 1.69; 95% CI: 1.05 - 2.73; P = 0.030) and end-stage renal disease (OR: 3.29; 95% CI: 1.93 - 5.62; P < 0.001) increased odds of in hospital mortality.
 Click to view | Table 4. Multivariate Analysis for In-Hospital Mortality |
| Discussion | ▴Top |
There are few studies to evaluate an association between classic IC and cirrhosis. Most of the literature and case studies of IC in the setting of cirrhosis surround phlebosclerotic colitis and right-sided colopathies [3]. Our study is significant in that the pathophysiology of cirrhosis may predispose the colon to ischemic insult and could bode as a marker for worse outcomes in patients with classic IC.
Although there have been other studies examining prognostic factors in IC, such as the ischemic colitis mortality risk (ICMR) score [7-10], none have included cirrhosis or portal hypertension as a potential prognostic or risk factor. This is despite some studies that suggest higher serum albumin, which is deranged in cirrhosis, is associated with survival benefit [10].
Even when adjusted for age, gender, race and co-morbid conditions, our study showed patients with IC and cirrhosis had a statistically significant increased mortality rate when compared to patients without cirrhosis. Presence of cirrhosis is associated with a greater than three-fold increased odds of in-hospital mortality. This compounds the already high rates of mortality in patients that undergo surgery for IC, up to 54% in some studies, and could be a reflection of lack of reserve to withstand the ischemic episode in the setting of cirrhosis [11-16].
With increased mortality we would have expected in-hospital colectomy rates also to be higher in the IC with cirrhosis group; however, colectomy rates were actually lower, though this was not significant when adjusted for age, gender, race and co-morbidities. Understanding that cirrhosis increases overall perioperative mortality, Child-Pugh class and model for end-stage liver disease score were not used to categorize surgical risk or severity of cirrhosis, and therefore appropriateness of surgery was not evaluated in this study due to its retrospective nature. It is plausible that surgical risk assessment may have affected colectomy rates for IC in the setting of cirrhosis despite possibly worse severity with concurrent diseases, but this would need to be studied further, ideally in a prospectively designed study. Colectomy rates overall were low for both IC with cirrhosis, and IC without cirrhosis groups (2.3% and 5.1%, respectively), which is keeping with prior meta-analyses and reviews, as non-occlusive IC is predominantly managed medically in about 80% of cases [14-16]. It is important to note that occlusive or non-occlusive etiologies and severity of IC were not factored into this study.
Patients with IC and cirrhosis had higher total hospital charges and longer LOS when compared to those without cirrhosis. This may reflect need for additional consultants and/or surgical or endoscopic intervention, if performed, in these complicated patients. Any procedure would be expected to increase cost as well as LOS.
In examination of the populations affected, patients with both IC and cirrhosis were more likely to be younger at age of presentation compared to those without cirrhosis. Compared to patients without cirrhosis, patients with IC and cirrhosis were more likely to be male, black and Hispanic, although patients in both groups were predominantly White. In contrast, the population of cirrhosis in the USA trends toward male, non-Hispanic blacks and Mexican-Americans, and are of older age [17-19]; however, the population dynamics of cirrhosis continue to change over time, and are expected to continue to do so, as rates of NASH and alcohol-related cirrhosis continue to increase and rates of hepatitis C-related cirrhosis decline [20].
Our study was hindered by multiple limitations. The first limitation is the retrospective design, which carries inherit weaknesses. Our study is constrained to patients with acute IC severe enough to be hospitalized and, thus, does not assess the full spectrum of disease. With the usually benign and transient nature of most IC cases, self-limited, symptomatic outpatient cases would not have been captured by our methodology.
Another limitation of our study is the nature of the NIS database itself. The NIS database only analyzes in-hospital mortality/cost/need for surgery for one admission, which can underestimate true mortality/cost/need for surgery. It is not possible to study prolonged periods, such as 30-, 60-, or 90-day mortalities. The database is limited to one principal diagnosis, and as such, may not capture patients with IC that were admitted for other more costly reasons.
Additionally, we rely on ascertainment of IC using diagnostic codes, without methods to confirm the diagnosis by reviewing histology or colonoscopy reports, which can potentially lead to misclassification bias. Considering the wide variation seen in presentations of IC, many cases of IC may be misdiagnosed with other conditions such as infectious colitis, inflammatory bowel disease, pseudomembranous colitis, diverticulitis and colon carcinoma [21, 22].
Despite these limitations, our study is derived from a large, robust and generalizable sample size with data from multiple hospitals nationwide. Single-institution studies are not easily generalized, making it important to evaluate this disease on national data. The volume of patients included in our study relative to previous reports in the literature provides important information for patients and clinicians. This analysis provides additional clinical guidance in predicting those at increased risk for increased mortality due to IC and may help establish realistic expectations with patients and their families.
In conclusion, we found that the presence of cirrhosis portends poorer outcomes in patients with IC. This was evidenced by an increased odds of in-hospital mortality and LOS but did not result in higher rates of in-hospital colectomy. Given these findings, patients with cirrhosis warrant closer observation. This is the first study that evaluated cost of this condition. We further advocate that any future research evaluate cost and also consider race as a prognostic indicator considering well-known healthcare disparities. This would allow us to better evaluate the societal impact of IC and cirrhosis and further aid in development of public health policy.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
For this type of retrospective database study, formal consent is not required.
Author Contributions
All authors certify that he or she has participated sufficiently in the intellectual content and the analysis of data. Each author has reviewed the final version of the manuscript and approves it for publication.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Naveau S, Bedossa P, Poynard T, Mory B, Chaput JC. Portal hypertensive colopathy. A new entity. Dig Dis Sci. 1991;36(12):1774-1781.
doi pubmed - Misra V, Misra SP, Dwivedi M, Singh PA, Kumar V. Colonic mucosa in patients with portal hypertension. J Gastroenterol Hepatol. 2003;18(3):302-308.
doi pubmed - Kang HY, Noh R, Kim SM, Shin HD, Yun SY, Song IH. Phlebosclerotic colitis in a cirrhotic patient with portal hypertension: the first case in Korea. J Korean Med Sci. 2009;24(6):1195-1199.
doi pubmed - Plackett TP, Coviello LC, Belnap CM, Phillips KJ, Gagliano RA, Sims CA. Intussusception and colonic ischemia in portal hypertension: a case report. Hawaii Med J. 2010;69(2):39-41.
- Khalifa A, Rockey DC. Lower gastrointestinal bleeding in patients with cirrhosis-etiology and outcomes. Am J Med Sci. 2020;359(4):206-211.
doi pubmed - HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2019. Agency for Healthcare Research and Quality, Rockville, MD.
- Reissfelder C, Sweiti H, Antolovic D, Rahbari NN, Hofer S, Buchler MW, Weitz J, et al. Ischemic colitis: who will survive? Surgery. 2011;149(4):585-592.
doi pubmed - Ritz JP, Germer CT, Buhr HJ. Prognostic factors for mesenteric infarction: multivariate analysis of 187 patients with regard to patient age. Ann Vasc Surg. 2005;19(3):328-334.
doi pubmed - Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M, Roque-Castellano C, Hernandez-Romero JM. Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J Surg. 2006;30(8):1579-1585.
doi pubmed - Sitges-Serra A, Mas X, Roqueta F, Figueras J, Sanz F. Mesenteric infarction: an analysis of 83 patients with prognostic studies in 44 cases undergoing a massive small-bowel resection. Br J Surg. 1988;75(6):544-548.
doi pubmed - Noh M, Yang SS, Jung SW, Park JH, Im YC, Kim KY. Poor prognostic factors in patients who underwent surgery for acute non-occlusive ischemic colitis. World J Emerg Surg. 2015;10:12.
doi pubmed - Antolovic D, Koch M, Hinz U, Schottler D, Schmidt T, Heger U, Schmidt J, et al. Ischemic colitis: analysis of risk factors for postoperative mortality. Langenbecks Arch Surg. 2008;393(4):507-512.
doi pubmed - Genstorfer J, Schafer J, Kettelhack C, Oertli D, Rosenthal R. Surgery for ischemic colitis: outcome and risk factors for in-hospital mortality. Int J Colorectal Dis. 2014;29(4):493-503.
doi pubmed - FitzGerald JF, Hernandez Iii LO. Ischemic colitis. Clin Colon Rectal Surg. 2015;28(2):93-98.
doi pubmed - O'Neill S, Yalamarthi S. Systematic review of the management of ischaemic colitis. Colorectal Dis. 2012;14(11):e751-763.
doi pubmed - Ryoo SB, Oh HK, Ha HK, Moon SH, Choe EK, Park KJ. The outcomes and prognostic factors of surgical treatment for ischemic colitis: what can we do for a better outcome? Hepatogastroenterology. 2014;61(130):336-342.
- Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, Volk ML. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015;49(8):690-696.
doi pubmed - Flores YN, Yee HF, Jr., Leng M, Escarce JJ, Bastani R, Salmeron J, Morales LS. Risk factors for chronic liver disease in Blacks, Mexican Americans, and Whites in the United States: results from NHANES IV, 1999-2004. Am J Gastroenterol. 2008;103(9):2231-2238.
doi pubmed - Collaborators GBDC. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245-266.
doi - Orman ES, Roberts A, Ghabril M, Nephew L, Desai AP, Patidar K, Chalasani N. Trends in characteristics, mortality, and other outcomes of patients with newly diagnosed cirrhosis. JAMA Netw Open. 2019;2(6):e196412.
doi pubmed - Huerta C, Rivero E, Montoro MA, Garcia-Rodriguez LA. Risk factors for intestinal ischaemia among patients registered in a UK primary care database: a nested case-control study. Aliment Pharmacol Ther. 2011;33(8):969-978.
doi pubmed - Theodoropoulou A, Koutroubakis IE. Ischemic colitis: clinical practice in diagnosis and treatment. World J Gastroenterol. 2008;14(48):7302-7308.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


