| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 5, October 2023, pages 270-275
The Impact of COVID-19 on Outcomes of Ischemic Colitis: A Nationwide Retrospective Analysis
Humzah Iqbala, f, Rakahn Haddadinb, Patrick Zhangc, Hasib Haidaryd, Devang Prajapatie
aDepartment of Internal Medicine, University of California San Francisco, Fresno, CA, USA
bDepartment of Internal Medicine, Sunrise Health Graduate Medical Education Consortium, MountainView Hospital, Las Vegas, NV, USA
cCollege of Osteopathic Medicine, California Health Sciences University, Clovis, CA, USA
dCollege of Medicine, American University of Antigua, Osbourn, Antigua and Barbuda
eDepartment of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA, USA
fCorresponding Author: Humzah Iqbal, Department of Internal Medicine, University of California San Francisco, Fresno, CA 93701, USA
Manuscript submitted July 23, 2023, accepted September 11, 2023, published online October 21, 2023
Short title: COVID-19 and Ischemic Colitis Outcomes
doi: https://doi.org/10.14740/gr1660
| Abstract | ▴Top |
Background: Ischemic colitis is the most common presentation of mesenteric ischemia and is associated with significant morbidity and mortality. Coagulopathy has been associated with the development of ischemic colitis. Coronavirus disease 2019 (COVID-19) infection can lead to a variety of pathology and physiological derangements, including coagulopathy. Some case reports have described severe ischemic colitis in patients with COVID-19 infection. Our study aimed to elucidate the impact of COVID-19 infection on ischemic colitis outcomes.
Methods: Patients with a diagnosis of ischemic colitis were identified using the 2020 Nationwide Inpatient Sample (NIS). Patients were stratified based on the presence of COVID-19 infection. Data were collected regarding mortality, shock, blood transfusion, length of stay, hospital charges, age, gender, race, primary insurance, median income, hospital region, hospital bed size, and comorbidities. The relationship between COVID-19 and outcomes was analyzed using multivariate regression analysis.
Results: A total of 67,685 patients were included in the final analysis. COVID-19 was associated with an increased risk of in-hospital mortality (adjusted odds ratio (aOR): 4.006, P < 0.001), shock (aOR: 1.62, P = 0.002), and blood transfusion (aOR: 1.49, P = 0.007). COVID-19 was also associated with an increased length of stay (16.2 days vs. 8.7 days) and higher total hospital charges ($268,884.1 vs. $145,805.9).
Conclusions: Among hospitalized patients with ischemic colitis, COVID-19 infection was associated with worse outcomes and higher resource utilization. Further studies are needed to investigate the mechanisms underlying this association.
Keywords: COVID-19; Ischemic colitis; Outcomes
| Introduction | ▴Top |
The coronavirus disease 2019 (COVID-19) pandemic was declared in March 2020 and was an unprecedented global health crisis. The virus was found to have a variety of manifestations, which are not limited solely to the respiratory tract. In fact, up to 51% of cases can have gastrointestinal (GI) symptoms, which include vomiting, diarrhea, and decreased appetite [1]. COVID-19 infection is also associated with coagulopathy secondary to severe inflammatory state and cytokine storm. Patients with COVID-19 infection are known to have elevated D-dimer and low fibrinogen levels [2]. COVID-19 hypercoagulability most commonly manifests as pulmonary embolism (PE) or deep venous thrombosis (DVT), however, it can also cause arterial thrombosis, microvascular thrombosis, and mesenteric ischemia [3].
Ischemic colitis is the most common form of mesenteric ischemia and was first described by Boley et al in 1963 [4]. It can be either occlusive or non-occlusive and most often affects the splenic flexure and sigmoid colon with rectal sparing due to being a watershed area with limited collateral blood supply [5]. Occlusive causes of ischemic colitis include mesenteric arterial thrombosis, emboli, or trauma. Non-occlusive ischemic colitis is most often seen in severe heart failure, perioperative hypotension, and hypovolemic or septic shock [6]. A prospective study by Midian-Singh et al identified hypercoagulability as a potential risk factor for ischemic colitis, and another study by Koutroubakis et al found the most significant associations with antiphospholipid antibodies and factor V Leiden mutations in particular [7, 8]. Ischemic colitis is known to have a high in-hospital mortality rate, with studies estimating from 11% to 29% [9-11]. Complications of ischemic colitis include bowel perforation, hemorrhage, peritonitis, and stricture formation [12]. The majority of patients are managed conservatively, though more severe cases may require surgical resection of the affected colonic segment [9].
Given its association with hypercoagulability and poor outcomes, we aimed to determine if COVID-19 infection plays a role in the hospital course and overall healthcare burden of patients admitted with ischemic colitis.
| Materials and Methods | ▴Top |
Data source
The National Inpatient Sample (NIS) is the largest database of inpatient hospital admissions in the United States [13]. It is maintained and operated by the Healthcare Cost and Utilization Project (HCUP) and is a 20% stratified sample of nationwide hospitalizations. The NIS is considered to be a validated and reliable estimation of hospitalization data including disease burden and outcomes. All patient information for each hospitalization is de-identified, therefore Institutional Review Board (IRB) approval was not required for this study.
Ethical compliance with human study
This study was performed in compliance with the Helsinki Declaration regarding research involving human subjects.
Study population
NIS was queried using the Internal Classification of Diseases 10th Version, Clinical Modification (ICD-10 CM) codes. Patients who were hospitalized with a diagnosis of ischemic colitis in 2020 were identified. A total of 69,340 patients were identified, of which 1,655 were missing mortality or demographic information and were excluded from the study. A total of 67,685 patients were included. Patients were then stratified into two groups based on the presence or absence of COVID-19 infection. The exclusion process and stratification of the final study population is outlined in Figure 1.
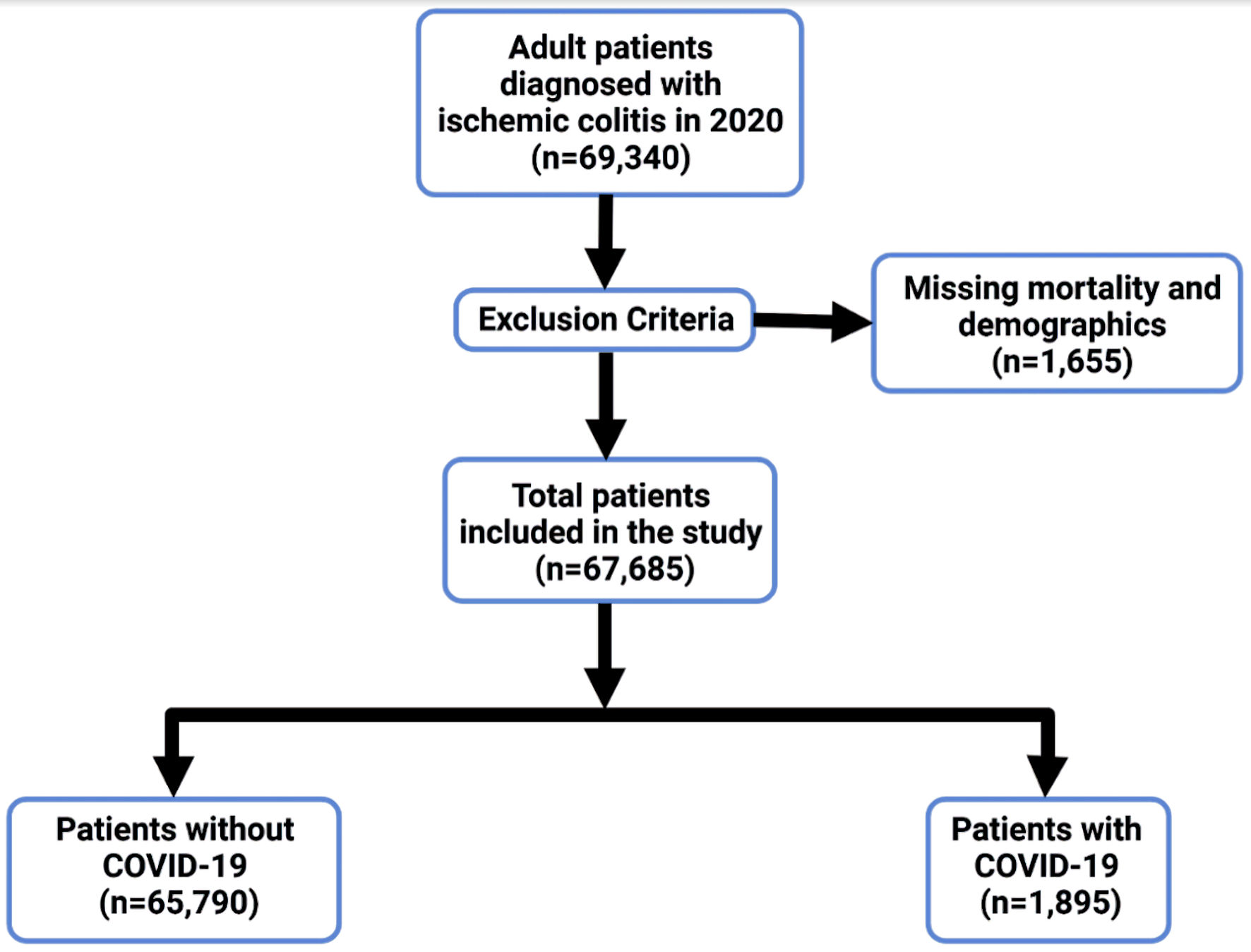 Click for large image | Figure 1. Flow diagram of inclusion and exclusion criteria for patients with ischemic colitis. COVID-19: coronavirus disease 2019. |
Study outcomes and variables
The primary study outcome was the impact of COVID-19 infection on in-hospital mortality in patients hospitalized with ischemic colitis. Secondary outcomes included shock, blood transfusion, mean length of stay (LOS), and total hospitalization charges.
Our primary exposure variable was the presence of COVID-19. Other variables included in our analysis were age, gender, race, primary insurance, median income, hospital region, and hospital bed size. The Charlson Comorbidity Index was used to assess comorbidities and predict mortality and resource use based on ICD-10 CM codes.
Statistical analysis
National estimates were generated using hospital-level discharge weights which were provided by NIS. Continuous variables were compared using an independent sample t-test. Categorical variables were compared using the Chi-square test. Univariate logistic regression was performed to elucidate the association between our variables and outcomes. We subsequently performed multivariate regression analysis while adjusting for variables with P < 0.1 on univariate analysis. The adjusted odds ratio (aOR) was obtained with a 95% confidence interval (CI). A type I error of < 0.05 was considered statistically significant.
| Results | ▴Top |
Patient characteristics
A total of 69,340 patients were hospitalized with ischemic colitis in the United States in 2020. Of these, 1,655 were missing data. A total of 67,685 patients were included in the study. Approximately 1,895 (2.8%) also had a diagnosis of COVID-19 infection while 65,790 (97.2%) did not. There was no difference in the average age of patients with ischemic colitis in the COVID-19 group and the non-COVID-19 group. The majority of patients in the COVID-19 group were White (55%), had Medicare insurance (66.7%), and three or more comorbidities (63.6%). Full demographic information of included subjects is outlined in Table 1.
 Click to view | Table 1. Patient Characteristics |
Outcomes
Total in-hospital mortality was 12,840 (19%). The mortality rate in the non-COVID-19 group was 18.2% compared to 47.2% in the COVID-19 group. The risk of mortality in patients with ischemic colitis was increased in the COVID-19 group with an aOR of 4.006 (P < 0.001) on multivariate analysis. A total of 5,144 patients in our study population developed shock (7.6%). Incidence of shock was 7.5% in the non-COVID-19 group compared to 12.1% in the COVID-19 group (P < 0.001). COVID-19 infection was associated with an increased risk of shock, with an aOR of 1.62 (P = 0.002) on multivariate analysis. Blood transfusion was required in a total of 7,648 patients (11.3%). Approximately 11.1% of patients in the non-COVID-19 group required blood transfusion compared to 16% in the COVID-19 group (P = 0.0045). On multivariate analysis, COVID-19 infection carried an increased risk for requiring blood transfusion during hospitalization with an aOR of 1.49 (P = 0.007). The mean LOS was 8.7 days in the non-COVID-19 group compared to 16.2 days in the COVID-19 group. Ischemic colitis patients without COVID-19 had a mean hospitalization charge of $145,805.9 compared to $268,884.1 in those with COVID-19. The association between outcomes and COVID-19 is outlined in Table 2.
 Click to view | Table 2. Multivariate Regression Analysis Showing Association Between COVID-19 and Categorical Outcomes |
| Discussion | ▴Top |
While there have been some case studies looking at the relationship between COVID-19 infection and ischemic colitis, there has been limited research on the true healthcare burden placed on GI complications stemming from COVID-19-induced coagulopathy secondary to causing a severe inflammatory state and cytokine storm. In our study, using data from the 2020 NIS patient database of nearly 69,000 patients during the initial wave of the pandemic with a diagnosis of ischemic colitis, we found an increased mortality rate in patients with COVID-19 and ischemic colitis (47.2%) versus ischemic colitis alone (18.2%). After adjusting for confounding factors, the odds ratio for mortality was found to be 4.006 (P < 0.001). These results indicate a substantially higher risk of death among patients with ischemic colitis and COVID-19 infection, emphasizing the detrimental effect of COVID-19 on this population. These results highlight the importance of proper preventative measures and diligent management of all patients with COVID-19 infection. Additional preventative measures for ischemic colitis such as but not limited to proper diet orders, intravenous (IV) fluids and early detection and patient education on signs of bowel discomfort could lead to early intervention, which may in turn lead to lower mortality rates. Patients with known risk factors such as age > 60, chronic renal disease/hemodialysis, atherosclerotic vascular disease/procedures, history of myocardial infarction, and history of acquired or hereditary thrombotic conditions should be evaluated with increased caution [14, 15].
One of the severe complications associated with a diagnosis of ischemic colitis is shock, which is characterized by inadequate tissue perfusion. Our study found that 7.5% of patients without COVID-19 infection developed shock, while the proportion increased to 12.1% in patients with COVID-19 infection (P < 0.001). Though shock is a known risk factor for the development of ischemic colitis, this suggests that COVID-19 infection may contribute to an elevated risk of shock development in patients with ischemic colitis. This finding could be explained by the overall derangement of other organ systems and pro-inflammatory state seen in COVID-19 [16]. A limitation of our study is that the NIS database does not allow for differentiation between whether ischemic colitis was caused by thrombosis or hypoperfusion due to shock, and further studies are needed to assess the etiology of ischemic colitis in COVID-19 patients.
Our study also assessed the need for blood transfusion in patients with ischemic colitis. Among those without COVID-19 infection, 11.1% required blood transfusions, while the proportion rose to 16% in patients with COVID-19 infection (P = 0.0045). These findings indicate a higher demand for blood transfusion in patients with COVID-19 and ischemic colitis, which may be attributed to the severity of presentation when both conditions are present concurrently, or potential complications associated with COVID-19 infection. It remains unclear whether subsequent variants of COVID-19 are also associated with an increased need for blood transfusion, and future studies are needed to evaluate this.
Patients with COVID-19 infection and ischemic colitis had a longer mean LOS, averaging 16.2 days compared to 8.7 days for patients without COVID-19 infection. The prolonged hospital stay can be partially attributed to quarantine rules and the need for closer monitoring and management of COVID-19-related symptoms. Consequently, patients with COVID-19 and ischemic colitis incurred higher mean total hospital charges of about $269,000 compared to $146,000 for those without COVID-19. These increased costs highlight the additional burden imposed by COVID-19 infection on the healthcare system.
Our study has several limitations. Given the features of the NIS data used in the study, illness scores of systemic inflammatory response syndrome (SIRS) and sepsis criteria were not able to be calculated. Additionally, cause of death is not known. This eliminates the ability to discern whether patients with COVID-19 are more likely to develop more severe ischemic colitis due to sepsis and hypotension from COVID-19, or if they are more likely to die from COVID-19-related pulmonary complications, since ischemic colitis can be a marker of poor cardiopulmonary status. Another potential error that could occur from data gathering using NIS is hospital readmissions, which could not be tracked. Documentation of diagnoses in the USA for in-hospital visits are documented using ICD-10 codes, this in turn could lead to coding errors in the form of incorrect input of ICD-10 codes and missed ischemic colitis ICD-10 codes when diagnosis is appropriate. The most recent dataset available from HCUP is NIS 2020, which contains information regarding the initial portion of the pandemic. Outcomes may differ when considering subsequent developments including vaccination, COVID-19 variants, and treatment regimens. We believe that the large population size and nationwide sample are significant strengths of our study and can help to mitigate the limitations. Despite lacking information regarding cause of death and outcomes in later waves of the pandemic, our study highlights a clear association between COVID-19 and worse outcomes in hospitalized patients with ischemic colitis. Further studies are needed in order to fully elucidate the true burden of COVID-19 on ischemic colitis outcomes and to outline the various mechanisms that may be at play in order to decrease the resulting morbidity, mortality, and healthcare burden.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
HI and RH were responsible for data collection, drafting of the manuscript, and approval of the final version to be published. PZ and HH were responsible for drafting the manuscript and approval of the final version to be published. DP was responsible for revising the manuscript for important intellectual content and approval of the final version to be published.
Data Availability
The authors declare that all data supporting the findings of this study are available within the article.
| References | ▴Top |
- Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, Li P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773.
doi pubmed pmc - Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, Pesenti A, et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738-1742.
doi pubmed pmc - Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L. The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management. Thromb Res. 2020;194:101-115.
doi pubmed pmc - Boley SJ, Schwartz S, Lash J, Sternhill V. Reversible vascular occlusion of the colon. Surg Gynecol Obstet. 1963;116:53-60.
pubmed - Theodoropoulou A, Koutroubakis IE. Ischemic colitis: clinical practice in diagnosis and treatment. World J Gastroenterol. 2008;14(48):7302-7308.
doi pubmed pmc - Green BT, Tendler DA. Ischemic colitis: a clinical review. South Med J. 2005;98(2):217-222.
doi pubmed - Midian-Singh R, Polen A, Durishin C, Crock RD, Whittier FC, Fahmy N. Ischemic colitis revisited: a prospective study identifying hypercoagulability as a risk factor. South Med J. 2004;97(2):120-123.
doi pubmed - Koutroubakis IE, Sfiridaki A, Theodoropoulou A, Kouroumalis EA. Role of acquired and hereditary thrombotic risk factors in colon ischemia of ambulatory patients. Gastroenterology. 2001;121(3):561-565.
doi pubmed - Gilshtein H, Hallon K, Kluger Y. Ischemic colitis caused increased early and delayed mortality. World J Emerg Surg. 2018;13:31.
doi pubmed pmc - Yadav S, Dave M, Edakkanambeth Varayil J, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sweetser SR, et al. A population-based study of incidence, risk factors, clinical spectrum, and outcomes of ischemic colitis. Clin Gastroenterol Hepatol. 2015;13(4):731-738.e731-736.
doi pubmed pmc - O’Neill S, Yalamarthi S. Systematic review of the management of ischemic colitis. Color Dis. 2012;14(11):751-763.
- Netz U, Galandiuk S. The management of ischemic colitis. In: Current surgical therapy 12th ed. Philadelphia: Elsevier; 2017. p. 171-176.
- Healthcare Cost and Utilization Project (HCUP) Content last reviewed October 2022 Agency for Healthcare Research and Quality, Rockville, MD. [Accessed November 14, 2022]. Available from: https://www.ahrq.gov/data/hcup/index.html.
- Diamond SM, Emmett M, Henrich WL. Bowel infarction as a cause of death in dialysis patients. JAMA. 1986;256(18):2545-2547.
pubmed - Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Iannaccone L, Dandrea G, Ames PR, et al. High prevalence of thrombophilic genotypes in patients with acute mesenteric vein thrombosis. Am J Gastroenterol. 2001;96(1):146-149.
doi pubmed - Dallan C, Romano F, Siebert J, Politi S, Lacroix L, Sahyoun C. Septic shock presentation in adolescents with COVID-19. Lancet Child Adolesc Health. 2020;4(7):e21-e23.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


