| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 3, June 2023, pages 141-148
Clinical Outcomes and Complications for Achalasia Patients Admitted After Per-Oral Endoscopic Myotomy
Dushyant Singh Dahiyaa, l , Fnu Niveditab, Abhilash Perisettic, Hemant Goyalb, Sumant Inamdard, Manesh Kumar Gangwanie, Muhammad Azizf, Hassam Alig, Chin-I Chengh, Madhusudhan R. Sanakai, Mohammad Al-Haddadj, Neil R. Sharmaj, k
aDepartment of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI, USA
bSection of Endoluminal Surgery and Interventional Gastroenterology, McGovern Medical School and UT Health Sciences Center at UT Health Houston, Houston, TX, USA
cDivision of Gastroenterology and Hepatology, Kansas Veterans Affairs Medical Centre, Kansas City, MO, USA
dDepartment of Gastroenterology and Hepatology, University of Arkansas for Medical Sciences, Little Rock, AR, USA
eDepartment of Internal Medicine, The University of Toledo Medical Center, Toledo, OH, USA
fDivision of Gastroenterology and Hepatology, The University of Toledo Medical Center, Toledo, OH, USA
gDepartment of Internal Medicine, East Carolina University, Greenville, NC, USA
hDepartment of Statistics, Actuarial and Data Science, Central Michigan University, Mt Pleasant, MI, USA
iDepartment of Gastroenterology, Hepatology and Nutrition, Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH, USA
jDivision of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN, USA
kInterventional Oncology & Surgical Endoscopy Programs (IOSE), Parkview Health, Fort Wayne, IN, USA
lCorresponding Author: Dushyant Singh Dahiya, Central Michigan University College of Medicine, Saginaw, MI 48603, USA
Manuscript submitted March 25, 2023, accepted May 13, 2023, published online June 11, 2023
Short title: Outcomes and Complications of POEM
doi: https://doi.org/10.14740/gr1617
| Abstract | ▴Top |
Background: Per-oral endoscopic myotomy (POEM) is a rapidly emerging minimally invasive procedure for management of achalasia. Same-day discharge after POEM is safe and feasible; however, some patients may need hospitalization. We aimed to identify characteristics and outcomes for achalasia patients requiring hospitalizations after POEM in the United States (US).
Methods: The US National Inpatient Sample was utilized to identify all adult achalasia patients who were admitted after POEM from 2016 to 2019. Hospitalization characteristics and clinical outcomes were highlighted.
Results: From 2016 to 2019, we found that 1,885 achalasia patients were admitted after POEM. There was an increase in the total number of hospitalizations after POEM from 380 in 2016 to 490 in 2019. The mean age increased from 54.2 years in 2016 to 59.3 years in 2019. Most POEM-related hospitalizations were for the 65 - 79 age group (31.8%), females (50.4%), and Whites (68.4%). A majority (56.2%) of the study population had a Charlson Comorbidity Index of 0. The Northeast hospital region had the highest number of POEM-related hospitalizations. Most of these patients (88.3%) were eventually discharged home. There was no inpatient mortality. The mean length of stay decreased from 4 days in 2016 to 3.2 days in 2019, while the mean total healthcare charge increased from $52,057 in 2016 to $65,109 in 2019. Esophageal perforation was the most common complication seen in 1.3% of patients.
Conclusion: The number of achalasia patients needing hospitalization after POEM increased. There was no inpatient mortality conferring an excellent safety profile of this procedure.
Keywords: Per-oral endoscopic myotomy; Achalasia; Outcomes; Mortality; Costs
| Introduction | ▴Top |
Achalasia is a rare chronic neurodegenerative motility disorder of the esophagus resulting in ineffective lower esophageal sphincter (LES) relaxation and peristalsis leading to progressive dysphagia [1]. The annual prevalence rate of achalasia is estimated to be 9 per 100,000 persons worldwide [2]. The exact etiology implicated in the development of achalasia is unknown but is believed to be of multi-factorial origin [2]. From a pathophysiological standpoint, patients with achalasia have inflammation and degeneration of the myenteric plexus resulting in the loss of inhibitory neurons [3]. This ultimately leads to an imbalance between the inhibitory (nitric oxide) and excitatory (acetylcholine) neurons with subsequent loss of relaxation of the LES and impaired peristalsis [4]. Patients with achalasia may present with a wide variety of clinical symptoms, progressive dysphagia being the most prominent, which leads to significant impairment in functional status and overall decreased quality of life [5, 6]. Management is primarily focused on reducing the LES hypertonicity by pharmacological, endoscopic, or surgical interventions [7].
Per-oral endoscopic myotomy (POEM) is a relatively recent minimally invasive endoscopic procedure used in the management of patients with achalasia [8, 9]. Since its inception in Japan in 2008, it has been endorsed by the American Society for Gastrointestinal Endoscopy (ASGE) in clinical practice [9]. POEM is performed by submucosal tunnel creation, and selective myotomy of the muscularis propria layer after a mucosal incision, decided on a case-by-case basis, proximal to the esophagogastric junction (EGJ) [10]. Recent studies have demonstrated that the short-term curative efficacy rate of POEM is > 90% [10-13]. Furthermore, clinical success rates of POEM at 12, 24 and 36 months have been estimated to be 92.9%, 90.6% and 88.4% respectively [14]. From an adverse event perspective, a study by Nino-Ramirez et al compared POEM to conventional treatments of achalasia such as laparoscopic Heller’s myotomy (LHM) and endoscopic balloon dilation (EBD) [15]. The authors reported that the proportion of adverse events was 3.6% for POEM, 4.9% for LHM, and 3.1% for EBD [15].
Multiple studies have been published on POEM; however, most of these studies are small or single-center experiences. At a national level, there is a significant knowledge gap on the outcomes and healthcare utilization by achalasia patients who underwent POEM and required hospitalization, as most of these patients are usually discharged the same day or after a 23-h observation period. Hence, this study aimed to investigate hospitalization characteristics, healthcare utilization, and clinical outcomes of POEM for achalasia patients that required hospitalization. Furthermore, we also estimated the rates of the common complications associated with the procedure.
| Materials and Methods | ▴Top |
Design and data source
The study population was extracted from the National Inpatient Sample (NIS) database, a part of the Healthcare Cost and Utilization Project (HCUP) databases by the Agency for Healthcare Research and Quality (AHRQ). The NIS is a large, all-payer, multi-ethnic database derived from collection of billing data submitted by United States (US) hospitals to state-wide data organizations covering > 95% of the US population [16]. It approximates a 20% stratified sample of discharges from US community hospitals. The data are further weighted to obtain national estimates. For the 2016 - 2019 study period, the NIS database was coded using the International Classification of Diseases Tenth Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS).
Study population
We identified all adult (≥ 18 years) achalasia patients who underwent POEM from January 1, 2016 to December 31, 2019.
Statistical analysis and outcome measures
The statistical analysis was conducted using SAS 9.4 (SAS Institute Inc., Cary, NC). A weighted sample was used during the statistical estimation process by incorporating variables for strata, cluster, and weight to discharges in the NIS database. Descriptive statistics were identified, including mean (standard error) for continuous variables and count (percentage) for categorical variables.
Ethical considerations
The NIS database contains numerous safeguards to protect patient privacy. It also lacks patient- and hospital-specific identifiers. Therefore, our study was exempt from Institutional Review Board (IRB) evaluation as per guidelines put forth by our institutional IRB for analysis of HCUP databases. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Hospitalizations characteristics
A total of 1,885 achalasia patients who underwent POEM required hospitalization during the 2016 - 2019 study period. There was an overall annual increase in the total number of these hospitalized patients from 380 in 2016 to 490 in 2019, without a statistically significant trend (Fig. 1). The mean age for these patients increased from 54.2 (± 1.4) years in 2016 to 59.3 (± 2.0) years in 2019. Females made up 50.4% of the study cohort. For the study period, the 65 - 79 age group had the highest proportion (31.8%) of patients, followed by the 50 - 64 and the 35 - 49 age groups (Table 1). A White (68.4%) predominance was also noted for the study period (Table 1). From a comorbidity perspective, a majority (56.2%) of the study population had a Charlson Comorbidity Index (CCI) of 0, while only 10% of the study cohort had a CCI score ≥ 3, representing selective patient cohort (Table 1).
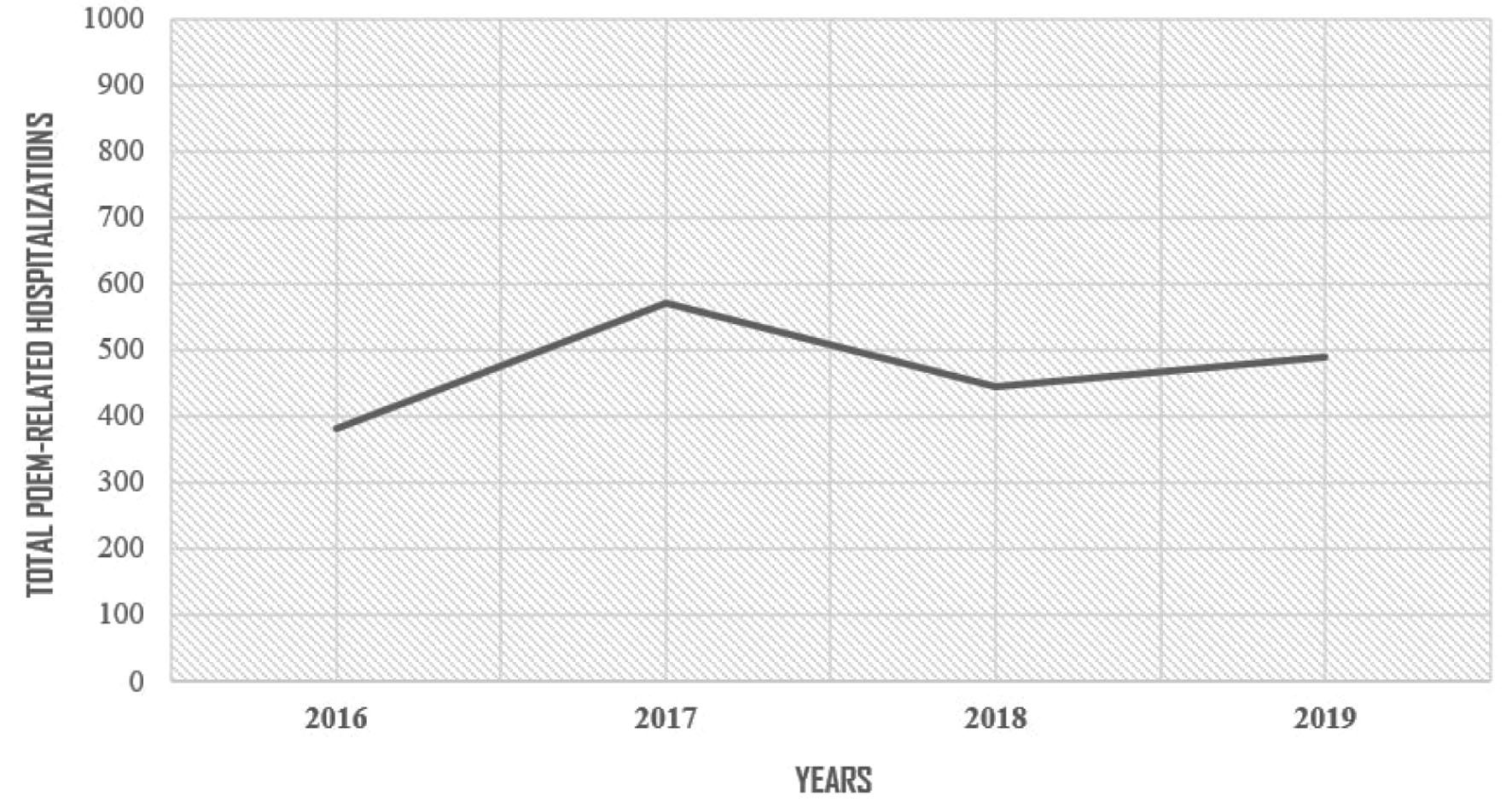 Click for large image | Figure 1. Achalasia patients requiring hospitalizations after per-oral endoscopic myotomy (POEM) in the United States from 2016 to 2019. |
 Click to view | Table 1. Hospitalization Characteristics for Patients With Achalasia That Underwent POEM in the Unites States From 2016 to 2019 |
Regional and hospital distribution
Most (33.7%) hospitalizations for achalasia after POEM were at the hospitals in the Northeast region (Fig. 2). There was a substantial increase in POEM-related hospitalization from 21.1% in 2016 to 39.8% in 2019 in the Southern region (Table 1). As expected, most of these patients were at large (86.2%) and urban teaching (96.3%) hospitals as most POEMs are performed in large academic hospitals (Table 1). Medicare (43.8%) was the largest primary payer for the hospital charge.
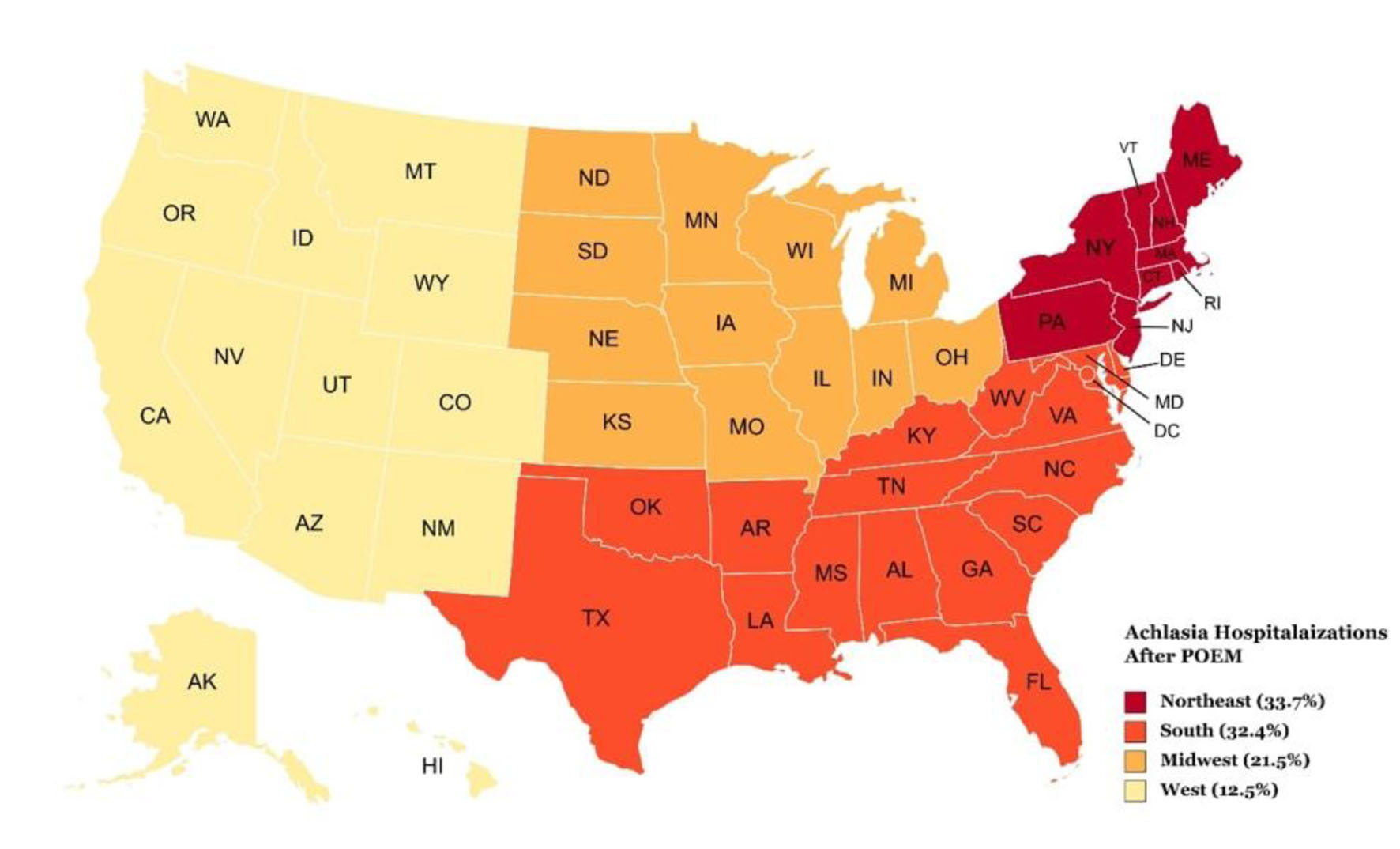 Click for large image | Figure 2. Geographical distribution of achalasia patients requiring hospitalizations after per-oral endoscopic myotomy (POEM) in the United States between 2016 and 2019. |
Clinical outcomes
Most of these patients (88.3%) were discharged home. There was no inpatient mortality from the procedure (Table 2). The average mean length of stay (LOS) was 3.7 days. Overall, the mean LOS decreased from 4 days in 2016 to 3.2 days in 2019. However, the mean total healthcare charge (THC) increased from $52,057 in 2016 to $65,109 in 2019.
 Click to view | Table 2. Trends of Outcomes for Patients With Achalasia That Underwent POEM in the Unites States From 2016 to 2019 |
Complications
Esophageal perforation was identified as the most common complication associated with the procedure and was seen in 1.3% of the study population (Table 2). Post-procedural pneumonia was seen in only 0.8% of all patients. Complications such as post-procedural hemorrhage and sepsis were not noted in the study cohort.
| Discussion | ▴Top |
POEM is used to treat a wide variety of esophageal motility disorders. This is the only study that evaluates hospitalization characteristics and outcomes for achalasia patients that were admitted after POEM in the USA using a national database. An understanding of data for those patients who required hospitalization post POEM is crucial as it provides endoscopists a better understanding of potential complications which needs to be recognized early and may lead to refinement of techniques or change in patient selection. In this study, we noted an overall increase in the number of admissions for achalasia patients who underwent POEM from 2016 to 2019. While the inpatient rate rose, likely so did national performance of POEM procedures. Esophageal perforation was the most common complication of the procedure but was seen only in a small proportion of patients, and no mortality was noted in the study.
The potential use of POEM for managing achalasia was first hypothesized in porcine animal models where endoscopic LES myotomy led to a significant fall in LES pressures [17]. Since its first utilization in patients with achalasia by Inoue et al, it has gained immense popularity and spread quickly worldwide to treat numerous esophageal motility disorders [18]. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has also issued strong recommendations for utilization of POEM in the management of achalasia [19]. In this study, we noted an overall increase in the total number of admissions for achalasia patients who underwent POEM from 380 in 2016 to 490 in 2019. However, it should be noted that a majority of the POEMs are performed at large urban teaching hospitals. This may partly be because these hospitals are usually tertiary care referral centres that are well equipped with the necessary resources and advanced endoscopists to perform this complex procedure. Furthermore, the Northeast hospital region had the highest proportion of hospitalizations of achalasia patients that underwent POEM (Table 1).
Literature reports that the mean age for patients with achalasia that undergo POEMs may range from 34 to 59 years, with a median age of approximately 51 years [20, 21]. The procedure has been established to be highly effective and safe in the elderly demographic, thereby increasing its utilization in the subset population [22, 23]. In our study, the mean age for achalasia patients that required hospitalization after POEM in the USA was 57.6 ± 0.9 years, with an increase in mean age for the 2016 - 2019 study period (Table 1). There was a substantial increase in the total number of POEM-related admissions from 90 in 2016 to 200 in 2019 for the 65 - 79 age group. Moreover, the 65 - 79 age group had the highest (31.8%) proportion of hospitalizations after POEM amongst all groups for the study period. These findings may be because endoscopists did not feel comfortable sending this older demographic home on the same day of the procedure. Additionally, the lack of immediate availability of a family caregiver at home may have also played a role. Interestingly, we also noted that 56.2% of all patients had a low comorbidity burden (CCI = 0). Furthermore, as with achalasia, studies on the utilization of POEM have not supported a specific gender predominance [20, 21, 24-26]. Similarly, in our study, a specific gender predominance was absent (Table 1). From a race perspective, much of our study cohort was White. This may be due to a higher overall number of achalasia patients of Caucasian background in the USA compared to other races [27].
Although the overall clinical success rate for POEM patients with achalasia ranges 82-100% and same-day discharge after a few hours of observation is feasible, there may be unplanned and prolonged hospitalizations in a minority of patients due to intra- or post-procedural complications [20, 28-33]. For our study cohort, the mean LOS in the hospital decreased from 4 days in 2016 to 3.2 days in 2019, indicating significant improvements in inpatient management strategies. There was no inpatient mortality related to the procedure during the study period. This is in agreement with current literature which reports no POEM-related deaths [11, 34, 35].
POEMs can be safely performed in an endoscopy suite as major adverse events are fairly uncommon, and patients usually tolerate the procedure well [36]. Early complications of the procedure include direct mucosal injury, intra- and post-procedural hemorrhage, esophageal perforation, pneumothorax, pneumomediastinum, pneumoperitoneum, aspiration pneumonia and subcutaneous emphysema [36, 37]. Gastroesophageal reflux and erosive esophagitis are late complications [38]. Most complications can be managed conservatively, with only a few requiring aggressive interventions. At a national level, esophageal perforation was the most common (1.3%) complication seen in these patients (Table 2). Post-procedural pneumonia was seen in 0.8% of all hospitalizations. We did not notice any cases of major post-procedural hemorrhage and sepsis in the study population. These low rates of complications associated with the procedure further reiterate its excellent safety profile.
POEM is a cost-effective procedure and is expected to continue to improve as familiarity and experience with the procedure increases [39]. However, in our study, the mean THC increased (Table 2). This may, in part, be attributed to increase in the total number of patients that were admitted after POEM and an increased healthcare utilization with the involvement of a multi-disciplinary team of specialists to manage these complex inpatient admissions. Additionally, the need for adequate training and maintenance of proficiency for POEM cannot be overemphasized. POEM continues to be a complex endoscopic procedure and due to the niche cohort of patients requiring POEM, reduction of cost is important. The best outcomes from the procedure are achieved with routine procedural performance in expert hands.
Our study has numerous strengths and limitations. A major strength of this study is the study population, which was obtained from one of the largest multi-ethnic databases available in the USA. An analysis over the 4-year study period allowed us to obtain meaningful information on characteristics and outcomes for achalasia patients who required hospitalization after POEM. Furthermore, as the NIS database covers greater than 95% of the US population, the results of our study are applicable to almost all achalasia hospitalizations that are managed with POEM in the USA, offering a national perspective on the procedure.
However, we do acknowledge all limitations associated with our study. As the ICD-10 procedure code for POEM is fairly recent, POEMs performed prior to the availability of the code may have been coded elsewhere, but the POEMs coded within the POEM procedure code are believed to be highly accurate. The NIS database does not contain information on the patients that were not admitted after POEM, time from hospitalization to discharge, hospital course, type/stage of achalasia treated, and other treatment aspects. It also lacks data on patient selection for the procedure, intra-procedural details, specific procedural techniques utilized during the procedure, operator preferences, and pharmacological aspects of management before, during or after the procedure. The study population was strictly limited to all achalasia patients who underwent POEM and were admitted after or specifically for the procedure. Additionally, the results of our study are not applicable to hospitalizations outside the USA. Furthermore, due to the retrospective nature of the study design, all biases associated with retrospective studies are applicable. Lastly, the NIS is an administrative database maintained through data collection organizations that use the ICD coding system to store inpatient data. Hence, the possibility of human coding errors cannot be excluded. However, despite these limitations, we believe that the large sample size and a comprehensive analysis technique help us better understand the characteristics, and outcomes of POEM for patients with achalasia in an inpatient setting.
Conclusion
There were 1,885 achalasia patients who underwent POEM that required hospitalization between 2016 and 2019 in the USA. These were mainly at large urban teaching hospitals as these larger centers have the necessary resources and expertise in performing this complex advanced procedure. Our study noted an expected rise in hospital charges during this period. The total number of achalasia patients that were admitted after POEM rose from 380 in 2016 to 490 in 2019 and 31.8% of them were in the 65 - 79 age group. This may be because endoscopists may not be comfortable sending these older patients home on the same day, or due to procedure-related complications emphasizing the need for extended training and maintenance of proficiency of the procedure through routine practice by subspecialized experts. Eventually, most of these patients were discharged home and there was no inpatient mortality highlighting the excellent safety profile of the procedure. In years to come, the trends of the utilization of POEM are expected to rise, and the focus on safety and same day discharge or observation may be one key measure of POEM quality.
Acknowledgments
None to declare.
Financial Disclosure
No funding sources to declare.
Conflict of Interest
All other authors report no conflict of interest.
Informed Consent
As the NIS database lacks patient and hospital identifiers, informed consent was not required for this study.
Author Contributions
Conceptualization: Dushyant Singh Dahiya, Mohammad Al-Haddad, and Neil R. Sharma. Data curation: Dushyant Singh Dahiya and Chin-I Cheng. Formal analysis: Chin-I Cheng. Investigation: all authors. Methodology: all authors. Project administration: Dushyant Singh Dahiya, Mohammad Al-Haddad, and Neil R. Sharma. Resources: Dushyant Singh Dahiya and Chin-I Cheng. Software: Chin-I Cheng. Supervision: Dushyant Singh Dahiya, Madhusudhan R. Sanaka, Mohammad Al-Haddad, and Neil R. Sharma. Validation: all authors. Visualization: all authors. Writing-original draft: all authors. Writing-review and editing: all authors.
Data Availability
The National Inpatient Sample (NIS) is a large, publicly available, all-payer inpatient care database in the United States containing data on millions of hospital stays per year. The large sample size derived from the NIS database provides sufficient data for the analysis of uncommon disorders and procedures. The NIS is publicly available at: https://www.hcup-us.ahrq.gov/.
Abbreviations
AHRQ: Agency for Healthcare Research and Quality; ASGE: American Society of Gastrointestinal Endoscopy; CCI: Charlson Comorbidity Index; EBD: endoscopic balloon dilation; EJG: esophagogastric junction; HCUP: Healthcare Cost and Utilization Project; ICD-10-CM/PCS: International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System; IRB: Institutional Review Board; LES: lower esophageal sphincter; LHM: laparoscopic Heller’s myotomy; LOS: length of stay; NIS: National Inpatient Sample; POEM: per-oral endoscopic myotomy; SAGES: Society of American Gastrointestinal and Endoscopic Surgeons; THC: total healthcare charge; US: United States
| References | ▴Top |
- Patel DA, Lappas BM, Vaezi MF. An overview of achalasia and its subtypes. Gastroenterol Hepatol (N Y). 2017;13(7):411-421.
pubmed pmc - O'Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19(35):5806-5812.
doi pubmed pmc - Ghoshal UC, Daschakraborty SB, Singh R. Pathogenesis of achalasia cardia. World J Gastroenterol. 2012;18(24):3050-3057.
doi pubmed pmc - Ates F, Vaezi MF. The pathogenesis and management of achalasia: current status and future directions. Gut Liver. 2015;9(4):449-463.
doi pubmed pmc - Patel DA, Vaezi MF. Achalasia and nutrition: is it simple physics or biology? Pract Gastroenterol. 2016;40:42-48.
- Nenshi R, Takata J, Stegienko S, Jacob B, Kortan P, Deitel W, Laporte A, et al. The cost of achalasia: quantifying the effect of symptomatic disease on patient cost burden, treatment time, and work productivity. Surg Innov. 2010;17(4):291-294.
doi pubmed - Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108(8):1238-1249.
doi pubmed - Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265-271.
doi pubmed - Gulati S, Emmanuel A, Inoue H, Hayee B, Haji A. Peroral endoscopic myotomy: a literature review and the first UK case series. Clin Med (Lond). 2017;17(1):22-28.
doi pubmed pmc - Kim JY, Min YW. Peroral endoscopic myotomy for esophageal motility disorders. Clin Endosc. 2020;53(6):638-645.
doi pubmed pmc - Li H, Peng W, Huang S, Ren Y, Peng Y, Li Q, Wu J, et al. The 2 years' long-term efficacy and safety of peroral endoscopic myotomy for the treatment of achalasia: a systematic review. J Cardiothorac Surg. 2019;14(1):1.
doi pubmed pmc - Khashab MA, Benias PC, Swanstrom LL. Endoscopic myotomy for foregut motility disorders. Gastroenterology. 2018;154(7):1901-1910.
doi pubmed - Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27(9):3322-3338.
doi pubmed - Ofosu A, Mohan BP, Ichkhanian Y, Masadeh M, Febin J, Barakat M, Ramai D, et al. Peroral endoscopic myotomy (POEM) vs pneumatic dilation (PD) in treatment of achalasia: A meta-analysis of studies with >/= 12-month follow-up. Endosc Int Open. 2021;9(7):E1097-E1107.
doi pubmed pmc - Nino-Ramirez S, Ardila O, Rodriguez FH, Londono J, Perez S, Sanchez S, Camargo J, et al. Major adverse events related to endoscopic or laparoscopic procedures in achalasia. A systematic review and meta-analysis. Rev Gastroenterol Mex (Engl Ed). 2023;88(1):36-43.
doi pubmed - Healthcare Cost and Utilization Project [database online]. Introduction to the HCUP National Inpatient Sample (NIS). The National (nationwide) Inpatient Sample database documentation. Rockville, MD: Agency for Healthcare Research and Quality; 2019. Accessed December 1, 2022.
- Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39(9):761-764.
doi pubmed - Cho YK, Kim SH. Current status of peroral endoscopic myotomy. Clin Endosc. 2018;51(1):13-18.
doi pubmed pmc - Kohn GP, Dirks RC, Ansari MT, Clay J, Dunst CM, Lundell L, Marks JM, et al. SAGES guidelines for the use of peroral endoscopic myotomy (POEM) for the treatment of achalasia. Surg Endosc. 2021;35(5):1931-1948.
doi pubmed - Xu J, Zhong C, Huang S, Zeng X, Tan S, Shi L, Peng Y, et al. Efficacy and safety of peroral endoscopic myotomy for sigmoid-type achalasia: a systematic review and meta-analysis. Front Med (Lausanne). 2021;8:677694.
doi pubmed pmc - Zhong C, Huang S, Xia H, Tan S, Lu M, Peng Y, Tang X. Role of peroral endoscopic myotomy in geriatric patients with achalasia: a systematic review and meta-analysis. Dig Dis. 2022;40(1):106-114.
doi pubmed - Okada H, Shiwaku H, Ohmiya T, Shiwaku A, Hasegawa S. Efficacy and safety of peroral endoscopic myotomy in 100 older patients. Esophagus. 2022;19(2):324-331.
doi pubmed - Li CJ, Tan YY, Wang XH, Liu DL. Peroral endoscopic myotomy for achalasia in patients aged >/= 65 years. World J Gastroenterol. 2015;21(30):9175-9181.
doi pubmed pmc - Mayberry JF. Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am. 2001;11(2):235-248.
pubmed - Eckardt VF, Hoischen T, Bernhard G. Life expectancy, complications, and causes of death in patients with achalasia: results of a 33-year follow-up investigation. Eur J Gastroenterol Hepatol. 2008;20(10):956-960.
doi pubmed - Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139(2):369-374.
doi pubmed - Wadhwa V, Thota PN, Parikh MP, Lopez R, Sanaka MR. Changing trends in age, gender, racial distribution and inpatient burden of achalasia. Gastroenterology Res. 2017;10(2):70-77.
doi pubmed pmc - Barbieri LA, Hassan C, Rosati R, Romario UF, Correale L, Repici A. Systematic review and meta-analysis: Efficacy and safety of POEM for achalasia. United European Gastroenterol J. 2015;3(4):325-334.
doi pubmed pmc - Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, et al. Per-oral endoscopic myotomy white paper summary. Surg Endosc. 2014;28(7):2005-2019.
doi pubmed - Benias PC, Korrapati P, Raphael KL, D'Souza LS, Inamdar S, Trindade AJ, Lee C, et al. Safety and feasibility of performing peroral endoscopic myotomy as an outpatient procedure with same-day discharge. Gastrointest Endosc. 2019;90(4):570-578.
doi pubmed - Cloutier Z, Mann A, Doumouras AG, Hong D. Same-day discharge is safe and feasible following POEM surgery for esophageal motility disorders. Surg Endosc. 2021;35(7):3398-3404.
doi pubmed - DiJoseph K, Manzo C, Pauli E, et al. Feasibility of Same Day Discharge Post-Peroral Endoscopic Myotomy. Dig Dis Interv. 2021;05:283-286.
- Tantau M, Crisan D. Peroral endoscopic myotomy: Time to change our opinion regarding the treatment of achalasia? World J Gastrointest Endosc. 2015;7(3):237-246.
doi pubmed pmc - Kohn GP. Peroral endoscopic myotomy for achalasia - a review. Ann Laparosc Endosc Surg. 2019;4:89.
- Raja S, Murthy SC, Tang A, Siddiqui HU, Parikh MP, Ahmad U, Gabbard S, et al. Per oral endoscopic myotomy: Another tool in the toolbox. J Thorac Cardiovasc Surg. 2019;158(3):945-951.
doi pubmed - Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018;87(1):4-17.
doi pubmed - Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery. 2013;154(4):893-897; discussion 897-900.
doi pubmed - Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy. 2016;48(12):1059-1068.
doi pubmed - Miller HJ, Neupane R, Fayezizadeh M, Majumder A, Marks JM. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc. 2017;31(4):1636-1642.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


