| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Case Report
Volume 11, Number 5, October 2018, pages 388-390
Esophageal Ulcers in Primary Biliary Cholangitis: A Rare Cause of Hematemesis in the Setting of Portal Hypertension and Esophageal Varices
Sindhura Kollia, c, Amit Moria, Isaac Moshenyatb
aDepartment of Gastroenterology and Hepatology, The Brooklyn Hospital Center, Academic Affiliate of The Icahn School of Medicine at Mount Sinai, Clinical Affiliate of The Mount Sinai Hospital, Brooklyn, NY, USA
bDepartment of Gastroenterology and Hepatology, New York University Langone Hospital-Brooklyn, Brooklyn, NY, USA
cCorresponding Author: Sindhura Kolli, 121 Dekalb Avenue, Brooklyn, NY 11201, USA
Manuscript submitted August 21, 2018, accepted September 17, 2018
Short title: Esophageal Ulcers in Primary Biliary Cholangitis
doi: https://doi.org/10.14740/gr1077w
| Abstract | ▴Top |
Our patient with primary biliary cholangitis, previously termed as primary biliary cirrhosis, presented with an unexpected and unusual cause of hematemesis in the form of multiple esophageal ulcers in-between variceal columns. Given that upon endoscopic examination, the esophageal ulcers were found to bleeding instead of the varices; they should be considered in the differential in the etiology of hematemesis in primary biliary cholangitis and thoroughly searched for during an endoscopic procedure for early treatment and subsequent secondary prevention.
Keywords: Primary biliary cirrhosis; Esophageal ulcers; Esophageal varices; Primary biliary cholangitis
| Introduction | ▴Top |
A classic case of esophageal varices in the setting of advanced primary biliary cholangitis (PBC), which was previously known as primary biliary cirrhosis, turned unusual when the sudden appearance of esophageal ulcers in-between the variceal columns were observed. While initially presumed to be endoscopic post-banding ligation ulcers, this patient never underwent an esophagogastroduodenoscopy (EGD), endoscopic banding, or sclerotherapy of her varices, having never experienced any symptoms from her advanced disease. This case report entails a previously unseen manifestation of PBC with portal hypertension and a new type of esophageal ulcer that should be explored as a possible alternate source of bleeding in PBC patients to expedite early recognition and treatment.
| Case Report | ▴Top |
We present a case of a 71-year-old Caucasian female patient with a past medical history of diabetes mellitus type 2, hypothyroidism, and hypertension presenting with symptoms of shortness of breath, abdominal distention and right lower leg edema that have been progressive in nature since beginning 2 months prior to admission. Ultrasound and transthoracic echocardiogram revealed a right-sided pleural effusion, pericardial effusion without tamponade, and moderate ascites contributing to her shortness of breath and abdominal distension as well as cirrhosis with liver nodularity and splenomegaly. A thoracentesis and interventional radiology (IR) guided paracentesis were done for both diagnostic and therapeutic purposes. Computed tomography angiography (CTA) and lower extremity venous Doppler were negative for pulmonary embolism and deep venous thrombosis, respectively. Initial laboratory workup showed normal aspartate aminotransaminase (AST) and alanine aminotransaminase (ALT) levels, but an elevated alkaline phosphatase (ALP) of 312 IU/L, slightly elevated gamma glutamyl-transferase (GGT) of 100 (IU/L), slightly elevated international normalized ratio (INR) of 1.2, decreased albumin of 2.4 g/dL and negative viral hepatitis panel. Her platelets, bilirubin and lactate dehydrogenase (LDH) were within normal limits. Further investigation revealed patient quit smoking 30 years prior, consumes 0 - 1 drinks per week, and never engaged in illicit drug usage. Ascitic fluid analysis from a paracentesis revealed a serum-ascites albumin gradient (SAAG) of > 1.2 g/dL and low protein suggestive of portal hypertension. Once positive antimitochondrial antibody (AMA) titer of 1.64 and a positive antinuclear antibodies (ANA) titer at 1.42 results returned, she was diagnosed with PBC and started on ursodiol and spironolactone. However, her hospital course became complicated with two episodes of hematemesis coffee ground emesis which required further investigation with an EGD.
EGD revealed cratered and linear ulcers with irregular shapes and blood intermittently oozing from the center in the esophagus in between > 5 mm non-bleeding esophageal varices in the middle and lower one third of the esophagus (Figs. 1, 2). Bipolar cautery was used successfully to halt bleeding from the ulcers. Octreotide drip was discontinued and a proton pump inhibitor (PPI) drip was continued which was later changed to oral. She had no more episodes of bleeding and discharged with appropriate outpatient follow-up with recommendations of non-selective beta blockers. Patient refused to have a repeat endoscopic evaluation of her esophageal ulcers.
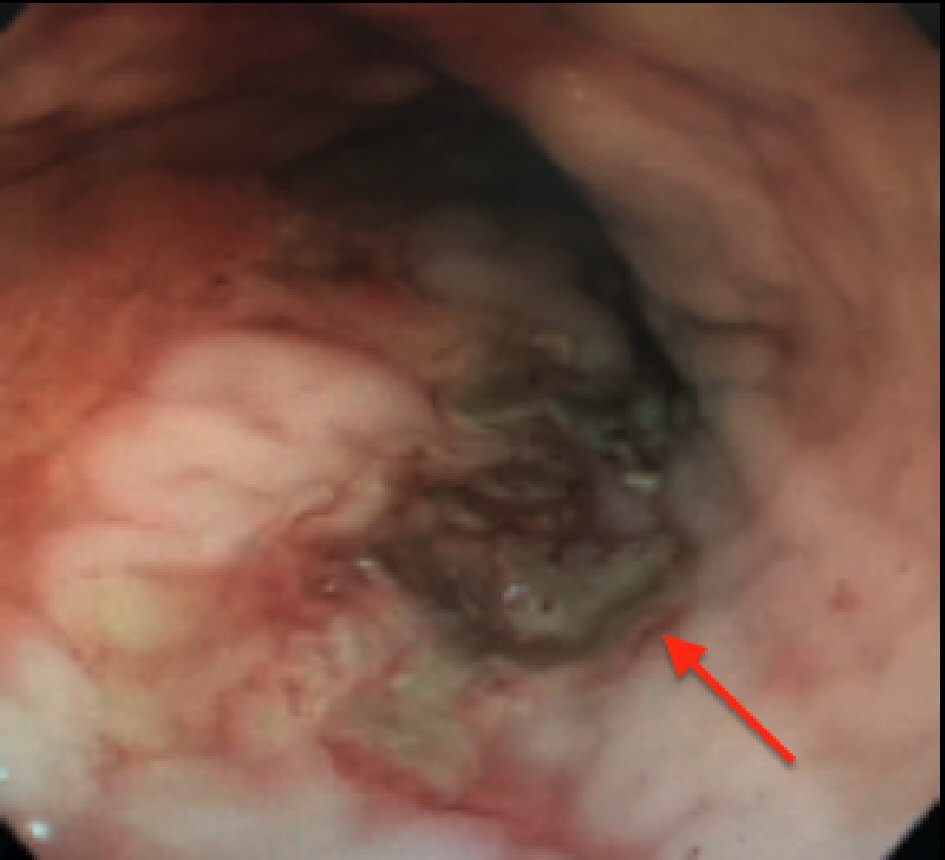 Click for large image | Figure 1. Ulcers in-between esophageal varices. |
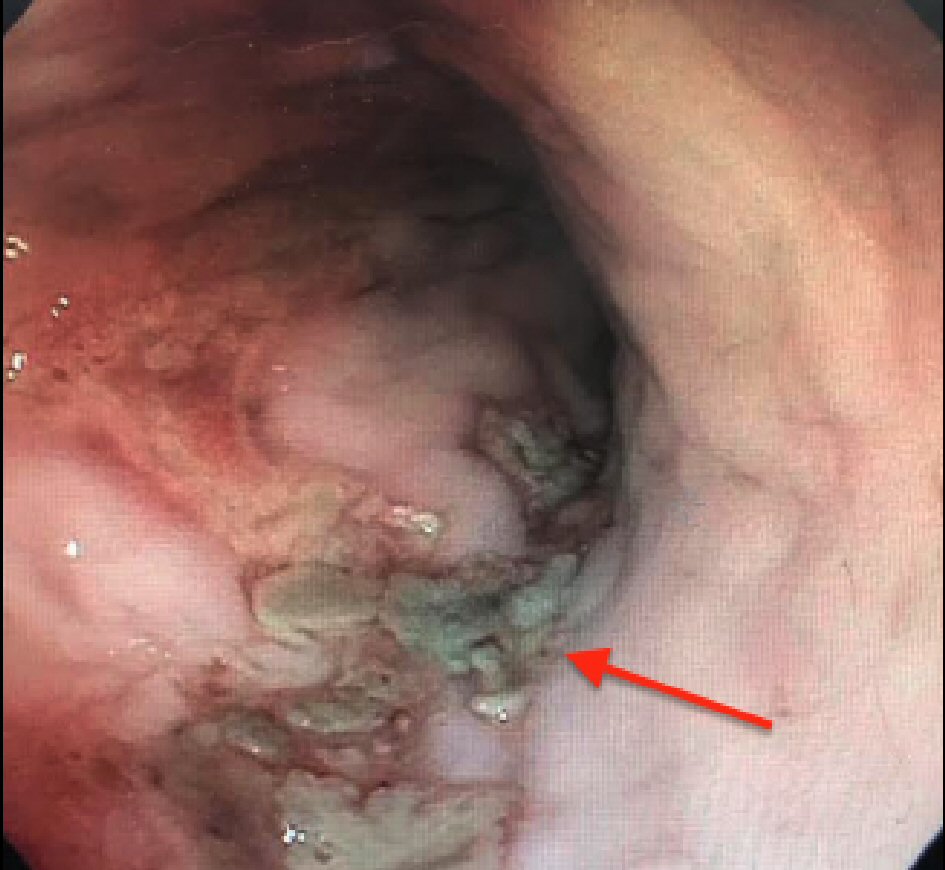 Click for large image | Figure 2. Esophageal ulcers and varices in primary biliary cholangitis. |
| Discussion | ▴Top |
To recognize the unusual nature of this case requires understanding the typical presentation of PBC. PBC is an autoimmune granulomatous disorder that destroys interlobular bile ducts leading to cholestasis that eventually becomes cirrhosis. Its target group is middle-aged Caucasian women similar to our patient. Typically, signs and symptoms of PBC include fatigue, jaundice, pruritus, elevated ALP, GGT, and total bilirubin with high titers of AMA present and sometimes ANA as well [1]. Patients also experience signs of portal hypertension such as ascites, splenomegaly, esophageal varices and hepatic encephalopathy, hepatopulmonary syndrome, hepatorenal syndrome [2]; however, nonvariceal bleeding in the presence of varices is extremely uncommon. Cirrhosis causing portal hypertension can cause abnormally enlarged and thickened submucosal veins known as varices. In events causing hemodynamic compromise such as hypovolemia, these thickened veins cannot compensate further as they have reached maximal dilatation and have minimal reserve, thus resulting in ischemia and necrosis of the mucosa creating ulcers. Varices are often treated by either sclerotherapy or more commonly, endoscopic band ligation (EBL). By placing a band on the bleeding tissue, blood supply is halted causing necrosis of the tissue and thrombosis of the varices. If the necrotic tissue is sloughed off, an ulcer will appear but heal within a few weeks. If the band falls off before the surrounding varices are thrombosed, the blood vessels will be exposed in this new ulcer and subsequently cause bleeding, known as post-banding ulcer hemorrhage (PBUH) which occurs up to 15% of EBL cases [3, 4]. This will manifest as hematemesis and increase mortality, length of stay, and readmission rates. However, our patient never had an EGD and never underwent EBL or sclerotherapy. She had unexpected and unusual cause of hematemesis in the form of multiple esophageal ulcers in-between variceal columns.
Additionally, our patient did not possess other risk factors involved in the development of esophageal ulcers. Broadly, ulcers can be divided into traumatic or iatrogenic, infectious or autoimmune. As mentioned earlier, she did not undergo endoscopic band ligation, sclerotherapy, no recent nasogastric tube placement, stress ulcers, and no caustic ingestion. She was not known for chronic non-steroidal anti-inflammatory drugs (NSAID) usage, which generally produces large shallow ulcers with normal surrounding mucosa or caustic antibiotic usage such as tetracyclines, which can leave behind circumferential ulcers that heal upon medication discontinuation [5]. Infectious processes such as cytomegalovirus (CMV) tend to imprint multiple, well-demarcated vertical/horizontal linear shallow ulcers, most commonly between the mid-third and lower-third areas of the esophagus [6]. Herpes simplex virus (HSV)-induced shallow erosive ulcers are similar to erosive reflux esophagitis and have a wider distribution pattern than CMV [6], while candidal white plaques will eventually give way to esophageal mucosal ulcers [7]. Gastroesophageal reflux disease (GERD)-induced esophageal ulcers are usually identified as superficial longitudinal ulcers and circumferential ulcers [8], while autoimmune processes like Behcet’s can rarely cause large, multiple, elliptical esophageal ulcers [9]. While our patient’s ulcer morphology most closely resembles that of post-endoscopic banding or sclerotherapy, she never underwent either procedure nor was she inflicted with any of the infectious, autoimmune or iatrogenic causes mentioned above. This diagnosis of exclusion leads us to suspect her esophageal ulcers were a result of her PBC. Given that upon endoscopic examination, the esophageal ulcers were found to bleeding instead of the varices, they should be considered in the differential as the etiology of hematemesis in primary biliary cirrhosis and thoroughly searched for during an endoscopic procedure for early treatment and subsequent secondary prevention.
Author Contributions
The above authors contributed equally and significantly to the concept and design, drafting, critical revision, and final approval of Introduction, Case Report and Discussion sections in the above titled case report.
Funding
This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors have no conflict of interest or financial relationships to disclose.
| References | ▴Top |
- Purohit T, Cappell MS. Primary biliary cirrhosis: Pathophysiology, clinical presentation and therapy. World J Hepatol. 2015;7(7):926-941.
doi pubmed - Patel A, Seetharam A. Primary Biliary Cholangitis: Disease Pathogenesis and Implications for Established and Novel Therapeutics. J Clin Exp Hepatol. 2016;6(4):311-318.
doi pubmed - Poza Cordon J, Froilan Torres C, Burgos Garcia A, Gea Rodriguez F, Suarez de Parga JM. Endoscopic management of esophageal varices. World J Gastrointest Endosc. 2012;4(7):312-322.
doi pubmed - Cho E, Jun CH, Cho SB, Park CH, Kim HS, Choi SK, Rew JS. Endoscopic variceal ligation-induced ulcer bleeding: What are the risk factors and treatment strategies? Medicine (Baltimore). 2017;96(24):e7157.
doi pubmed - Kim SH, Jeong JB, Kim JW, Koh SJ, Kim BG, Lee KL, Chang MS, et al. Clinical and endoscopic characteristics of drug-induced esophagitis. World J Gastroenterol. 2014;20(31):10994-10999.
doi pubmed - Bhaijee F, Subramony C, Tang SJ, Pepper DJ. Human immunodeficiency virus-associated gastrointestinal disease: common endoscopic biopsy diagnoses. Patholog Res Int. 2011;2011:247923.
- Takahashi Y, Nagata N, Shimbo T, Nishijima T, Watanabe K, Aoki T, Sekine K, et al. Long-term trends in esophageal candidiasis prevalence and associated risk factors with or without HIV infection: lessons from an endoscopic study of 80,219 patients. PLoS One. 2015;10(7):e0133589.
doi pubmed - Fukuda N, Ishimura N, Okada M, Izumi D, Mikami H, Okimoto E, Aimi M, et al. Mucosal breaks show same circumferential distribution in majority of patients with recurrent reflux esophagitis. Endosc Int Open. 2017;5(3):E214-E221.
doi pubmed - Fujiwara S, Shimizu I, Ishikawa M, Uehara K, Yamamoto H, Okazaki M, Horie T, et al. Intestinal Behcet's disease with esophageal ulcers and colonic longitudinal ulcers. World J Gastroenterol. 2006;12(16):2622-2624.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


