| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 1, February 2023, pages 37-49
Comparing Patients Diagnosed With Ineffective Esophageal Motility by the Chicago Classification Version 3.0 and Version 4.0 Criteria
Alyssa W. Tuana , Nauroz Syeda, Ronaldo P. Panganibana, Roland Y. Leea, Shannon Dalessioa, Sandeep Pradhanb, Junjia Zhub, Ann Ouyanga, c
aDepartment of Medicine, Pennsylvania State University College of Medicine, Hershey, PA 17033, USA
bDepartment of Public Health Sciences, Pennsylvania State University College of Medicine, Hershey, PA 17033, USA
cCorresponding Author: Ann Ouyang, Department of Medicine, Pennsylvania State University College of Medicine, PO Box 850, Hershey, PA 17033, USA
Manuscript submitted October 6, 2022, accepted November 7, 2022, published online February 28, 2023
Short title: Comparing Patients With IEM by CCv3.0 and CCv4.0
doi: https://doi.org/10.14740/gr1563
| Abstract | ▴Top |
Background: The Chicago Classification version 4.0 (CCv4.0) of ineffective esophageal motility (IEM) is more stringent than the Chicago Classification version 3.0 (CCv3.0) definition. We aimed to compare the clinical and manometric features of patients meeting CCv4.0 IEM criteria (group 1) versus patients meeting CCv3.0 IEM but not CCv4.0 criteria (group 2).
Methods: We collected retrospective clinical, manometric, endoscopic, and radiographic data on 174 adults diagnosed with IEM from 2011 to 2019. Complete bolus clearance was defined as evidence of exit of the bolus by impedance measurement at all distal recording sites. Barium studies included barium swallow, modified barium swallow, and barium upper gastrointestinal series studies, and collected data from these reports include abnormal motility and delay in the passage of liquid barium or barium tablet. These data along with other clinical and manometric data were analyzed using comparison and correlation tests. All records were reviewed for repeated studies and the stability of the manometric diagnoses.
Results: Most demographic and clinical variables were not different between the groups. A lower mean lower esophageal sphincter pressure was correlated with greater percent of ineffective swallows in group 1 (n = 128) (r = -0.2495, P = 0.0050) and not in group 2. In group 1, increased percent of failed contractions on manometry was associated with increased incomplete bolus clearance (r = 0.3689, P = 0.0001). No such association was observed in group 2. A lower median integrated relaxation pressure was correlated with greater percent of ineffective contractions in group 1 (r = -0.1825, P = 0.0407) and not group 2. Symptom of dysphagia was more prevalent (51.6% versus 69.6%, P = 0.0347) in group 2. Dysphagia was not associated with intrabolus pressure, bolus clearance, barium delay, or weak or failed contractions in either group. In the small number of subjects with repeated studies, a CCv4.0 diagnosis appeared more stable over time.
Conclusions: CCv4.0 IEM was associated with worse esophageal function indicated by reduced bolus clearance. Most other features studied did not differ. Symptom presentation cannot predict if patients are likely to have IEM by CCv4.0. Dysphagia was not associated with worse motility, suggesting it may not be primarily dependent on bolus transit.
Keywords: Chicago Classification v4.0; Chicago Classification v3.0; Deglutition disorders; Esophageal diseases; Esophageal motility disorders
| Introduction | ▴Top |
Ineffective esophageal motility (IEM) is a diagnosis made based on the vigor of contractions measured during swallows in patients who undergo high-resolution esophageal manometry (HRM) [1]. It was classified as a minor esophageal motor disorder under Chicago Classification version 3.0 (CCv3.0) [1]. As IEM was not consistently associated with specific esophageal symptoms and could also be seen in asymptomatic healthy individuals, the clinical significance of the finding was unclear [2].
Based on studies suggesting that failed contractions are more relevant to abnormal esophageal acid burden than weak contractions [3] and that increased proportions of failed contractions are better predictors of reflux burden and outcome [4], the criteria for making a manometric diagnosis of IEM were updated in December 2020. Under the Chicago Classification version 4.0 (CCv4.0), a diagnosis of IEM now requires ineffective contractions following > 70% of swallows or failed contractions following ≥ 50% of swallows on HRM study [5]. By contrast, the CCv3.0 definition only required ineffective contractions following ≥ 50% percent of swallows.
Our study aimed to determine the demographic and clinical differences between patients who meet the CCv4.0 criteria (group 1) compared to patients who only meet the CCv3.0 criteria (group 2) [1]. We also assessed for underlying medical conditions or medications more prevalent in either group. We hypothesized that patients meeting CCv4.0 criteria will have evidence of worse esophageal function as indicated by clearance and additional diagnostic studies.
| Materials and Methods | ▴Top |
Patient selection
This retrospective study included 201 adults who underwent HRM testing from January 1, 2011, to June 1, 2019, at the Milton S. Hershey Medical Center, and were diagnosed with IEM based on CCv3.0. A gastroenterologist specialized in motility disorders (AO) reviewed each manometric tracing to confirm the diagnosis. Study exclusions included: eight patients for a prior history of achalasia, five patients for missing comorbidity and medication data from the time of IEM diagnosis, five patients for technical failure or artifacts on HRM, and nine patients for integrated relaxation pressure (IRP) > 15. This left 174 patients remaining in the study. The 174 patients meeting inclusion criteria were categorized into two groups: 128 patients met both CCv3.0 and CCv4.0 IEM criteria and were placed in group 1; 46 patients met only CCv3.0, and not CCv4.0, IEM criteria (“CCv3.0 only patients”) and were placed in group 2. Institutional Review Board (IRB) approval was obtained for this study. Ethical standards for human and animal studies were not applicable to this study.
Data collection
Medical charts were manually reviewed, and baseline data from the time of diagnosis were collected. Collected data included demographics, symptoms, previous surgeries and endoscopic treatments, comorbidities from nine different body systems (Supplementary Material 1, www.gastrores.org), medications, alcohol and tobacco use, findings on HRM, upper endoscopy, and barium studies. Manometry studies were reviewed using the Medtronic ManoView software (Medtronic, Minneapolis, MN) for percent of weak and failed contractions. Weak contractions were defined as distal contractile integral (DCI) between 100 and 449 mm Hg s cm, whereas failed contractions were defined as DCI less than 100 mm Hg s cm [6]. Ineffective contractions are the sum of weak and failed contractions [1]. Additional manometric variables analyzed were lower esophageal sphincter (LES) pressure, IRP, intrabolus pressure, and incomplete bolus clearance [7, 8]. The bolus entry can be identified in the proximal esophagus. Complete bolus clearance was defined by the bolus exit occurring at all distal esophageal impedance recording sites. Failure of the bolus exit to be identified at all distal impedance recording sites was designated incomplete bolus transit.
Upper endoscopy studies were available for 103 patients in group 1 and 44 patients in group 2. Data collected from the reports included normal or abnormal esophageal and gastric findings, if biopsies had been taken, and, if so, the results of those biopsies. Barium studies were available for a portion of patients (n = 75 in group 1, n = 26 in group 2), as were pH impedance studies (n = 47 in group 1, n = 19 in group 2). Barium studies included barium swallow, modified barium swallow, and barium upper gastrointestinal series studies. Data were collected on whether esophageal dilation, abnormal stomach findings, diverticulum, abnormal motility, and delay in passage of liquid barium and barium tablet were noted in a study’s report. Data collected from pH impedance study reports included whether a study was performed on or off acid-reducing medications, percent of time that gastric and esophageal pH were below 4, number of acid and non-acid reflux episodes, and recorded symptoms.
Additionally, all available HRM studies performed before the IEM diagnosis and up to 3 years afterward were reviewed to study the stability of disordered peristalsis over time. Normal esophageal body function for this part of the study was defined by > 50% of swallows followed by normal contractions.
Study data were collected and managed using REDCap electronic data capture tools hosted at the Penn State College of Medicine [9, 10].
Statistical methods
Descriptive statistics were generated to summarize patients’ demographic and baseline clinical information. Categorical variables are summarized as frequencies and relative frequencies (n (%)), while quantitative variables are summarized as means ± standard deviations. Statistical comparisons between the two groups were performed using nonparametric Wilcoxon rank-sum tests, two-sample t-tests, or Fisher exact tests when appropriate. Spearman correlation coefficients (ρ) and the P-values for testing (ρ = 0) were reported to check the bivariate associations between some quantitative measures, for all patients’ records first and then stratified by groups. Analyses were performed using statistical software SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) [11]. All tests were two-sided using a statistical significance level of 0.05. Due to the exploratory nature of this study, significance level was not adjusted for multiple testing.
| Results | ▴Top |
Demographics
Table 1 summarizes demographics for groups 1 and 2, including age, gender, race, and body mass index (BMI), which were not significantly different.
 Click to view | Table 1. Frequency of Demographic and Clinical Characteristics Among CCv4.0 IEM Patients (n = 128) and CCv3.0 Only IEM Patients (n = 46), 2011 - 2019 |
Comorbidities
The conditions captured from the charts for each organ system are listed in Supplementary Material 1 (www.gastrores.org). Disorders of the digestive system, endocrine system, and mood were most prevalent in both groups. Their prevalence, however, were not statistically different between groups 1 and 2 (Table 1). Blood and immune system disorders, which include anemia and sarcoidosis, were more prevalent in group 2 (13.3% vs. 30.4%, P = 0.0132). The prevalence of other disorders by body system category studied was not different statistically.
Within the digestive system disorders, gastroesophageal reflux disease (GERD) and hiatal hernia were most prevalent in both groups 1 and 2 (Fig. 1) and not significantly different. Barrett’s esophagus was not more prevalent in either group.
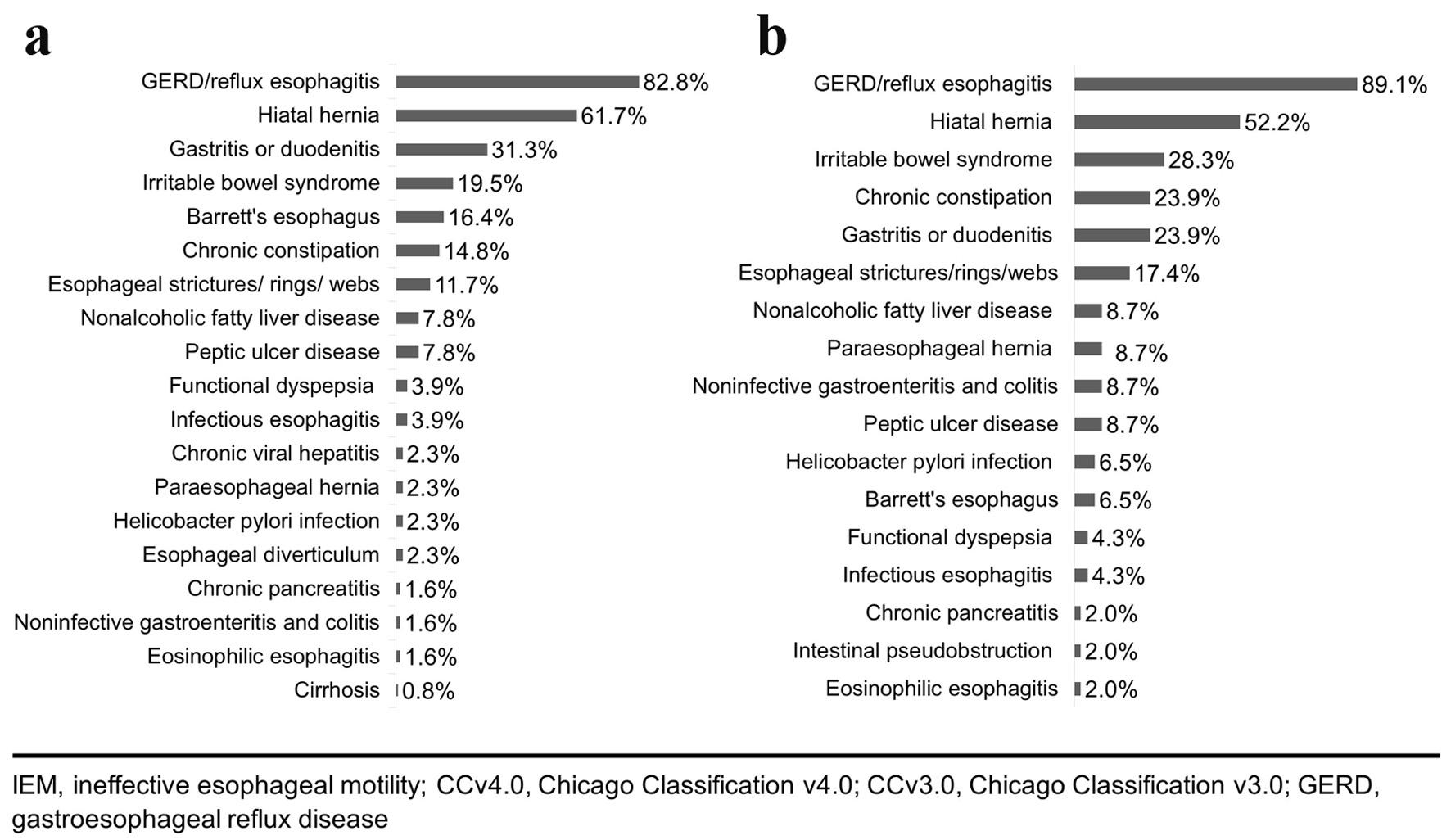 Click for large image | Figure 1. Prevalence of specific digestive system disorders among patients with a digestive system comorbidity among: (a) CCv4.0 IEM patients (n = 128) and (b) CCv3.0 only IEM patients (n = 46), 2011 - 2019. |
History of any alcohol or tobacco use was not different between groups 1 and 2.
Medications
The medications used by patients in groups 1 and 2 are shown in Figure 2. The most common medication classes used were proton pump inhibitor (PPI), selective serotonin reuptake inhibitor or serotonin and norepinephrine reuptake inhibitor (SSRI/SNRI), and non-steroidal anti-inflammatory drug (NSAID) in both groups 1 and 2 (Fig. 2). There were no significant differences among the distributions of these medication classes between the two groups. Diuretics were more common in group 1 (23.4% vs. 6.5%, P = 0.0146), whereas beta-adrenergic antagonists were more common in group 2 (14.2% vs. 28.9%, P = 0.0424).
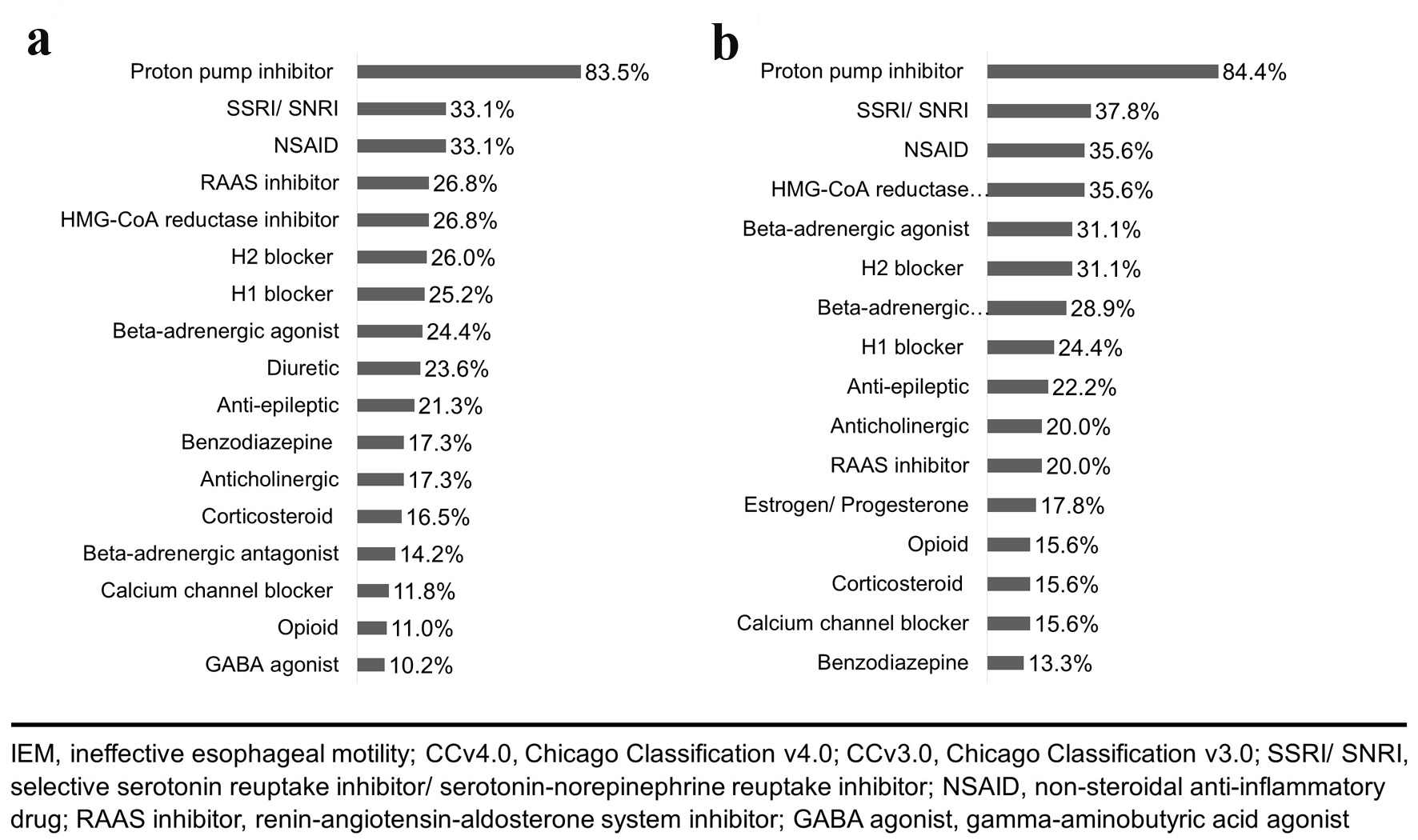 Click for large image | Figure 2. Prevalence of medication classes used by: (a) CCv4.0 IEM patients (n = 128) and (b) CCv3.0 only IEM patients (n = 46), 2011 - 2019. |
The association of medications on manometry parameters was examined on all patients combined. Usage of SNRIs, SSRIs, benzodiazepines, or beta-adrenergic agonists was not associated with mean LES pressure, DCI, median IRP, or percent of weak, failed, or ineffective contractions. Fourteen patients in group 1 and seven patients in group 2 were taking opioids. Irrespective of their group classification, opioid use was associated with lower mean LES pressure compared to patients not using the medication (13.0 ± 8.2 mm Hg vs. 19.8 ± 13.2 mm Hg, P = 0.0069). Opioids were also associated with lower median IRP (1.6 ± 5.4 mm Hg vs. 4.4 ± 5.9 mm Hg, P = 0.0435). Calcium channel blocker use (15 patients in group 1 and seven patients in group 2) was associated with greater percent of weak contractions (51.2 ± 22.5% vs. 39.9 ± 26.5%, P = 0.0493).
Symptoms
In groups 1 and 2, the top symptom documented in the patient chart for a visit that led to the manometry study was dysphagia (51.6% vs. 69.6%, P = 0.0347), which was more prevalent in group 2. Other common symptoms included reflux, regurgitation, and heartburn, which were not significantly different between the two groups.
HRM findings
Table 2 details the average manometric findings for groups 1 and 2. As expected, based on the definition of the groups, there was a significant difference for mean percent of failed contractions (46.6 ± 25.9% vs. 19.2 ± 15.0%, P < 0.001) and mean percent of ineffective contractions (87.9 ± 11.9% vs. 60.8 ± 8.2%, P < 0.001).
 Click to view | Table 2. Average Manometric Findings Among CCv4.0 IEM Patients (n = 128) and CCv3.0 Only IEM Patients (n = 46), 2011 - 2019 |
For group 1, an inverse correlation was noted between mean LES pressure and percent of effective swallows (DCI ≥ 450 mm Hg s cm) (r = -0.2495, P = 0.0050) (Table 3, Fig. 3b, d), with no relationship in group 2. A correlation persisted when patients from both group 1 and group 2 were analyzed together (Table 3, Fig. 3f). On the other hand, mean LES pressure was not associated with percent of failed contractions (DCI < 100 mm Hg s cm) in group 1 (Table 3, Fig. 3a), while they were associated in group 2 (r = -0.4875, P < 0.001) (Table 3, Fig. 3c).
 Click to view | Table 3. Correlation of Mean LES Pressure and Median IRP With Percent of Failed and Ineffective Contractions Among CCv4.0 IEM Patients (n = 128), CCv3.0 Only IEM Patients (n = 46), and All Patients Combined (n = 174), 2011 - 2019 |
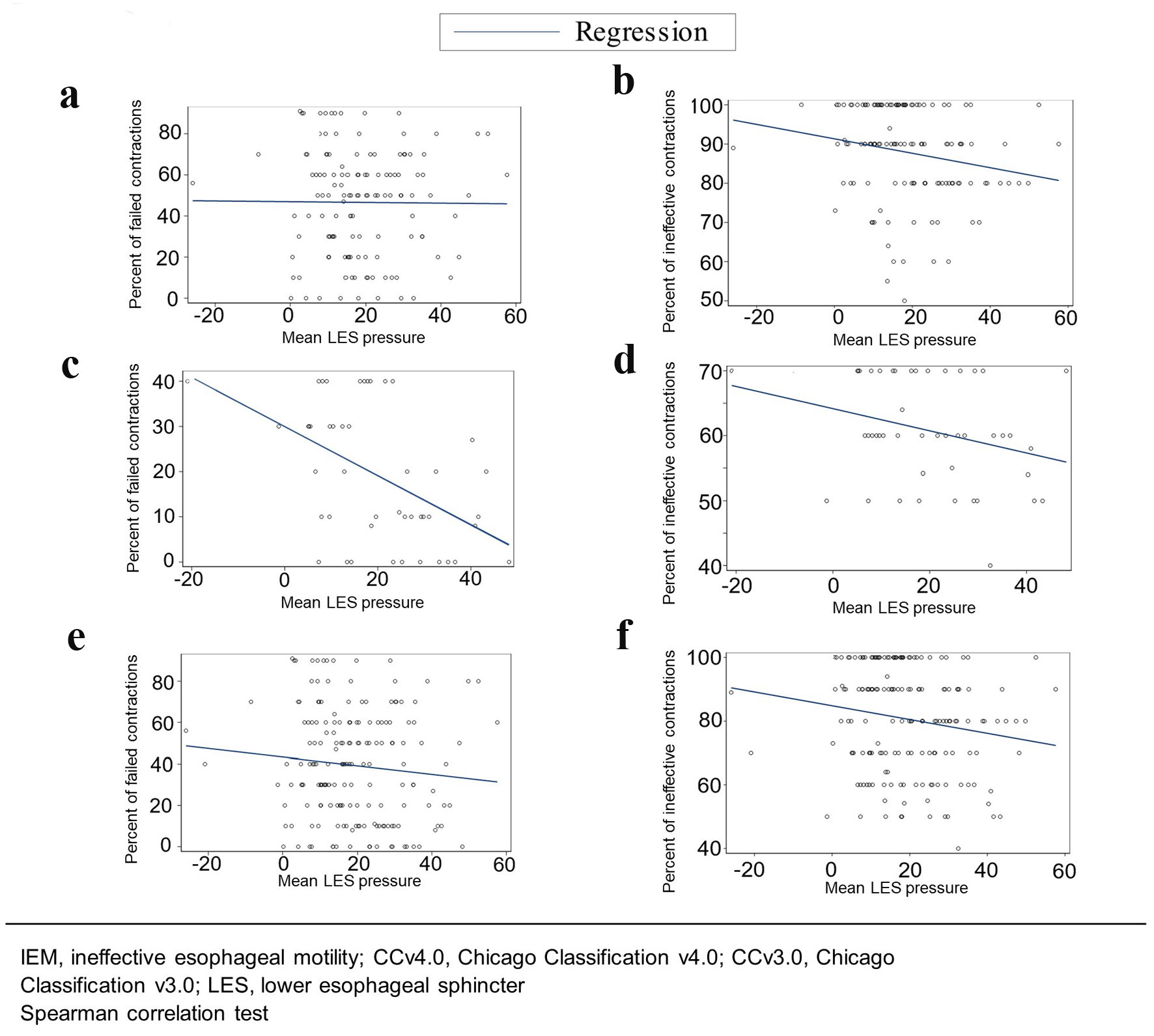 Click for large image | Figure 3. Correlation of mean LES pressure with: (a) Percent of failed contractions among CCv4.0 IEM patients (n = 128) (r = -0.0409, P = 0.6473), (b) Percent of ineffective contractions among CCv4.0 IEM patients (n = 128) (r = -0.2495, P = 0.0050), (c) Percent of failed contractions among CCv3.0 only IEM patients (n = 46) (r = -0.4875, P < 0.001), (d) Percent of ineffective contractions among CCv3.0 only IEM patients (n = 46) (r = -0.2954, P = 0.0507), (e) Percent of failed contractions in all patients combined (n = 174) (r = -0.1172, P = 0.1249), and (f) Percent of ineffective contractions in all patients combined (n = 174) (r = -0.1942, P = 0.0108). |
Mean LES pressure was not associated with symptom of dysphagia, reflux, or regurgitation or upper endoscopy finding of hiatal hernia or esophagitis in group 1 or 2 (Supplementary Material 2, www.gastrores.org).
The IRP is a metric used to assess the adequacy of LES relaxation at the esophagogastric junction. Median IRP was not different between groups 1 and 2 (Table 2) and was not correlated with incomplete bolus clearance (Supplementary Material 3, www.gastrores.org). Median IRP was inversely correlated with percent of ineffective contractions in group 1 (r = -0.1825, P = 0.0407) (Table 3, Fig. 4b), but not in group 2 or in all patients combined. Median IRP was inversely correlated with percent of failed contractions in group 2 (r = -0.3036, P = 0.0445) (Table 3, Fig. 4c) and in all patients combined (r = -0.1533, P = 0.0445) (Table 3, Fig. 4e), but not in group 1.
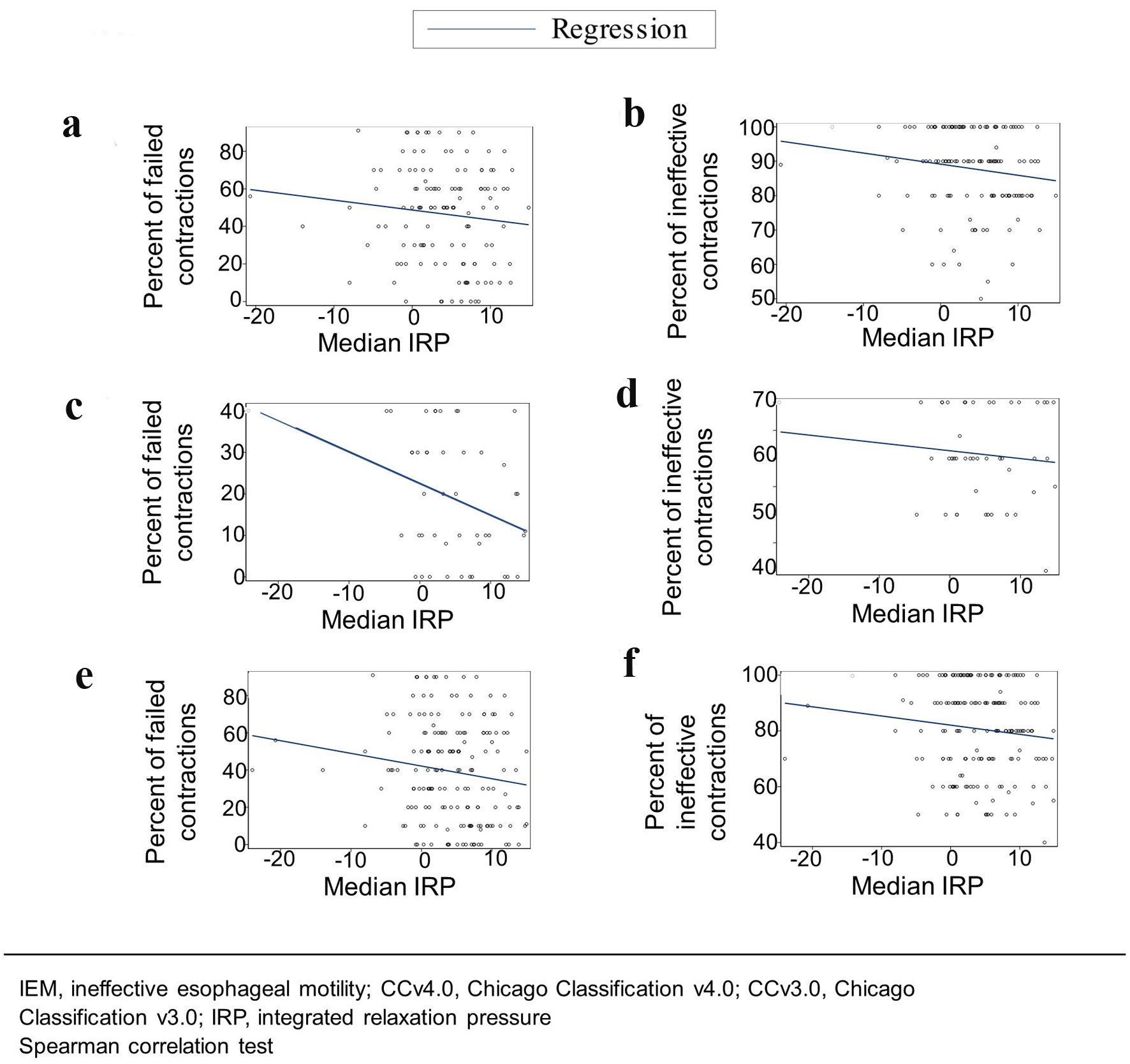 Click for large image | Figure 4. Correlation of median IRP with: (a) Percent of failed contractions among CCv4.0 IEM patients (n = 128) (r = -0.1202, P = 0.1785), (b) Percent of ineffective contractions among CCv4.0 IEM patients (n = 128) (r = -0.1825, P = 0.0407), (c) Percent of failed contractions among CCv3.0 only IEM patients (n = 46) (r = -0.3036, P = 0.0445), (d) Percent of ineffective contractions among CCv3.0 only IEM patients (n = 46) (r = -0.0587, P = 0.7000), (e) Percent of failed contractions in all patients combined (n = 174) (r = -0.1533, P = 0.0445), and (f) Percent of ineffective contractions in all patients combined (n = 174) (r = -0.1163, P = 0.1277). |
Bolus transit
In group 1, incomplete bolus clearance was correlated with decreased percent of weak contractions (r = -0.2707, P = 0.0054) (Table 4) and increased percent of failed contractions (r = 0.3689, P = 0.0001). These were not correlated in group 2. Similar to findings in group 1, when both groups are combined, there is a correlation between incomplete bolus clearance with decreased percent of weak contractions (r = -0.2176, P = 0.0081) and increased percent of failed contractions (r = 0.3859, P = 0.000002). Incomplete bolus clearance was not associated with percent of ineffective contractions (combined failed and weak contractions) in group 1 or group 2, but they were correlated among all patients combined (r = 0.2716, P = 0.0009).
 Click to view | Table 4. Correlation of Incomplete Bolus Clearance With Percent of Weak, Failed, and Ineffective Contractions Among CCv4.0 IEM Patients (n = 128), CCv3.0 Only IEM Patients (n = 46), and All Patients Combined (n = 174), 2011 - 2019 |
Barium study findings
Normal versus abnormal motility reported on barium study, liquid barium delay, barium tablet delay, and reflux on barium study were not associated with percent of weak, failed, or ineffective contractions on HRM in group 1 or group 2.
EGD and pH impedance study findings
No differences were seen between groups 1 and 2 in the prevalence of esophagitis and hiatal hernia found on upper endoscopy (Supplementary Material 4, www.gastrores.org). When comparing patients not on a PPI in group 1 (n = 9) versus group 2 (n = 2), there was no difference in abnormal esophageal pH exposure on pH impedance study. Among patients not on a PPI, there was also no correlation between abnormal pH exposure with percent of weak or failed contractions or mean LES pressure (Supplementary Material 5, www.gastrores.org). Abnormal pH exposure among people on a PPI was not different between patients in group 1 (51.7%, n = 29) versus group 2 (70.0%, n = 20) (P = 0.2464).
Association of dysphagia with esophageal function
Symptom of dysphagia was not associated with intrabolus pressure, incomplete bolus clearance, or barium tablet delay in either group. Among patients with dysphagia compared to those without dysphagia, there was no difference in terms of percent of weak or failed contractions.
Stability of manometric diagnoses among IEM patients with more than one HRM
Twenty-five patients underwent an additional HRM either before the IEM diagnosis or up to 3 years afterward. Sixteen patients had completed an additional study before the study HRM, and nine patients completed an additional study after the study HRM. Change in HRM diagnosis over time was recorded along with the interval between studies (Fig. 5). Frequencies of initial HRM diagnoses were: IEM CCv3.0 only and not CCv4.0 (CCv3.0) (n = 5), IEM CCv4.0 (n = 12), normal peristalsis (n = 6), and absent contractility (n = 2) (Fig. 6). Figure 6 displays the frequencies of the follow-up diagnosis and the mean between-study time interval in months including range. More patients diagnosed with IEM CCv4.0 maintained this diagnosis (75.0%, with an average 18 months (range: 4 - 55 months) between manometry diagnoses) over time compared to patients diagnosed with IEM CCv3.0 (20.0%, with 89 months between the diagnosis), although the difference was not statistically significant. Two patients with IEM CCv3.0 and four with IEM CCv4.0 had a prior study indicating normal peristalsis; the mean between-study time interval in months for these patients was 86 months (range: 33 - 138 months) for IEM CCv3.0 and 16 months (range: 6 - 32 months) for IEM CCv4.0. The most prevalent indication for follow-up HRM studies was dysphagia. Patients with normal peristalsis who converted to IEM typically had an initial HRM indication of dysphagia.
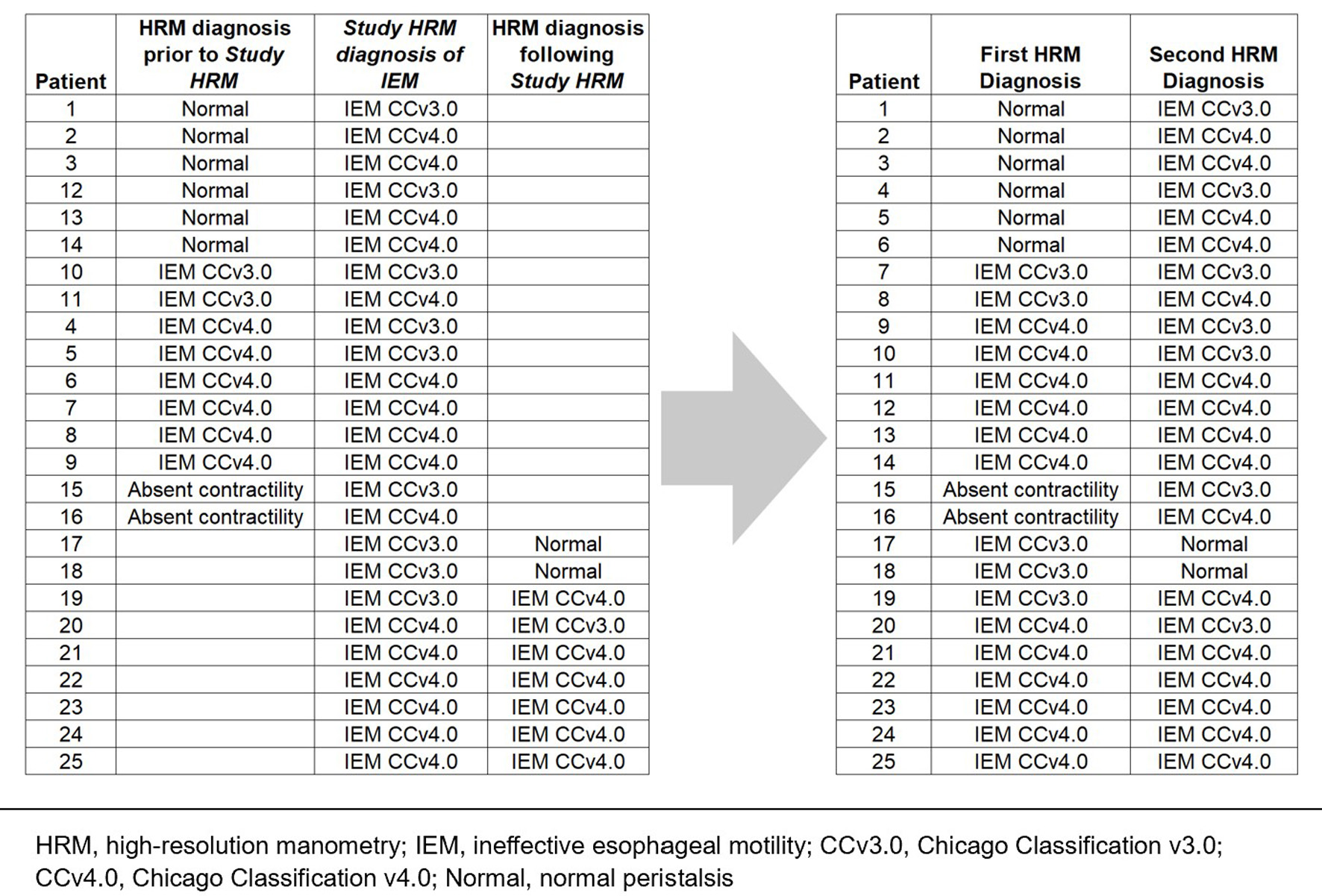 Click for large image | Figure 5. The conversion of HRM diagnoses from 25 patients from three separate time points - (1) HRM diagnosis prior to study HRM, (2) Study HRM diagnosis of IEM, and (3) HRM diagnosis following study HRM - into “first HRM diagnosis” and “second HRM diagnosis,” 2011 - 2019. |
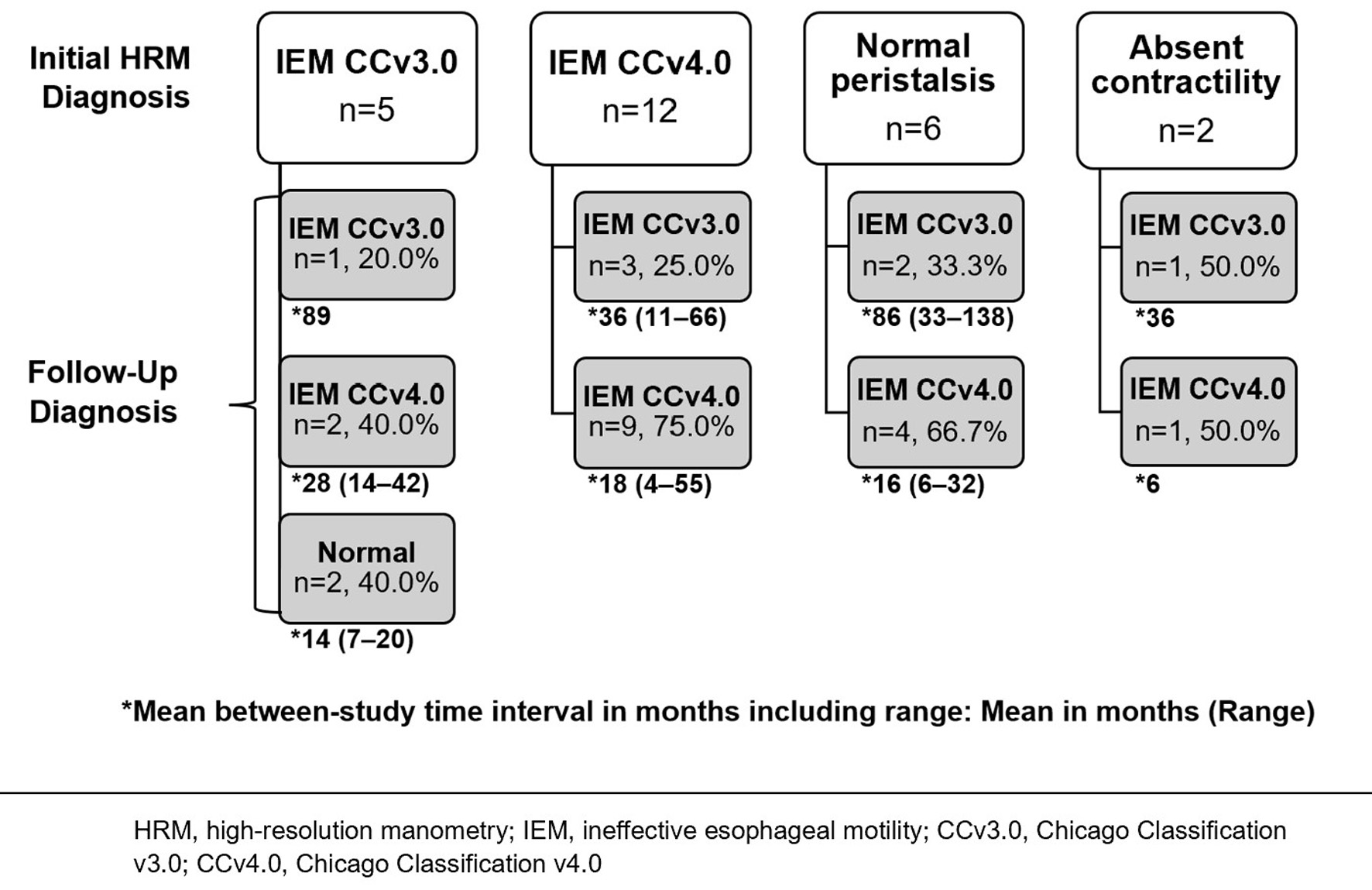 Click for large image | Figure 6. Frequency of initial and follow-up HRM diagnoses for patients diagnosed with IEM from 2011 to 2019 and with more than one HRM study (n = 25), including mean time interval in months (including range) between the initial and follow-up studies. |
Patients with an initial HRM diagnosis of IEM CCv4.0 had a borderline lower percent of peristalsis (55 ± 26% vs. 76 ± 15%, P = 0.057) and borderline higher percent of failed contractions (45 ± 25% vs. 24 ± 15%, P = 0.054) at the time of the study HRM compared to patients with an initial IEM CCv3.0 diagnosis, as expected based on definition.
| Discussion | ▴Top |
We analyzed the demographic, clinical, manometric, endoscopic, and radiographic data of patients who underwent HRM testing at the Hershey Medical Center from 2011 to 2019 and who met the IEM CCv4.0 criteria (group 1) or CCv3.0, and not CCv4.0, IEM criteria (group 2). Our aims were to identify if differences among these data between the two groups and whether underlying comorbidities or medications were more prevalent in group 1. At the time of this study, there had only been one published peer-reviewed study (n = 93) comparing the clinical characteristics of IEM patients by CCv3.0 and CCv4.0, and that study largely examined abnormal acid exposure [12]. A very recent publication showed that IEM was less frequent with CCv4.0 compared to CCv3.0, which is to be expected given the new criteria [13]. It also showed that the gastroesophageal reflux disease questionnaire (GerdQ) scores were higher for IEM by CCv4.0, with no difference in the Eckardt score or brief esophageal dysphagia questionnaire (BEDQ) noted. Our study found that: 1) Most demographic and clinical variables were not different between groups 1 and 2; 2) In group 2, blood and immune system disorders were more prevalent than in group 1. Diuretic medications were more commonly used in group 1, and beta-adrenergic antagonists were more prevalent in group 2; 3) A CCv4.0 IEM diagnosis was associated with more impaired bolus transit which may reflect worse esophageal function; 4) Symptom presentation cannot predict if patients are likely to have IEM by CCv4.0; and 5) Dysphagia was not associated with worse motility, suggesting that the symptom of dysphagia is not primarily dependent on bolus transit.
There was no statistical difference between groups 1 and 2 for many demographic and clinical factors examined, including age, gender, race, and BMI. The percent of obese patients in our study was similar to the prevalence of adult obesity in the USA [14]; thus, obesity likely did not contribute to our findings for IEM.
We expected GERD [2, 15, 16], symptom of reflux, and an upper endoscopy finding of esophagitis [17] to be more prevalent in CCv4.0 patients. We did not find a significant difference between groups 1 and 2 for these findings, suggesting that GERD, reflux, and esophagitis may not help distinguish between a patient with IEM meeting CCv3.0 versus CCv4.0 criteria. The vast majority of patients were on a PPI medication, and this may have affected findings, although abnormal pH exposure from pH impedance studies was not different between the groups when stratified by current or lack of PPI usage at the time of study.
Depression was surprisingly prevalent in our study and has been associated with gastrointestinal disorders such as GERD [18]. Depression may be mediated by poor sleep quality in the setting of GERD [19]. Antidepressant medication, commonly used among our study participants, could also impair esophageal motility. SNRIs have been associated with significantly higher resting LES pressure and increased DCI [20]. In our study, we did not find these associations for SNRIs nor SSRIs.
Several medications have been reported to impact smooth or skeletal muscle function, such as cyclobenzaprine, tizanidine, and baclofen [2, 21-23]. These medications were not prevalent among patients in our study. Although opioids have been described to increase IRP [24, 25], they were associated with lower mean LES pressure and lower median IRP in this study. The number of patients using opioids was low in this study population. In most studies, opioid use has been associated with hypercontractile changes, and IEM is diagnosed less frequently in patients on opioids [25]. The impact of opioids on patients who have IEM diagnosed has not been specifically examined. Our review also did not determine which opioids or dose of opioids were prescribed. Many patients were on several medications, which may also mitigate the effect of opioids. Calcium channel blockers were associated with greater percent of weak contractions. This finding is not unexpected, as calcium channel blockers have been used to treat hypercontractile esophagus due to their ability to reduce the amplitude of peristaltic contractions [26, 27]. NSAIDs, the third-most prevalent drug class in our study, have a known relationship in causing gastric ulcers and may aggravate an acid-related esophageal disease [28, 29]. However, there was no difference in the prevalence of calcium channel blocker, opioid, or NSAID use among groups 1 and 2, supporting the view that calcium channel blockers and opioids do not impact an IEM diagnosis [2]. A history of alcohol use was common in our studied population, and alcohol use can lead to esophageal dysfunction by increasing LES pressure or inhibiting smooth or striated muscle function [28]. However, although alcoholism with neuropathy has been associated with IEM [30], we did not observe any difference in a history of alcohol use compared to no history of use between groups 1 and 2.
Diuretics were more common in group 1; this is possibly because hypertension prevalence was 44.5% in group 1 compared to 37.0% in group 2, although this prevalence was not statistically different. Beta-adrenergic antagonists were more common in group 2; we noted that ischemic heart disease prevalence was 10.2% in group 1 and 19.6% in group 2. We are otherwise unable to draw significant conclusions on the contribution of comorbidities or medication usage to an IEM CCv4.0 diagnosis compared to an IEM CCv3.0 diagnosis, given that their prevalence was largely not different between the groups, and there were such a large range of multiple medications prescribed to these patients, raising the likelihood of confounders. A future analysis comparing an IEM CCv4.0 population with a control group may be helpful to identify the contribution of comorbidities and medication usage to an IEM diagnosis by the CCv4.0 criteria.
A CCv4.0 IEM diagnosis was associated with worse esophageal function as measured by bolus transit. Increased incomplete bolus clearance was correlated with increasing percent of failed contractions, consistent with previous studies [8, 31, 32]. As the percent of ineffective contractions ranges between 70% and 100% in group 1, an inverse relationship between the percent of failed contractions and that of weak contractions would be expected. These findings of esophageal dysfunction support the CCv4.0 update for IEM as identifying more clinically significant cases. These findings also indicate the value of obtaining a bolus impedance study to support an IEM diagnosis by the CCv4.0 criteria, consistent with other reports [5, 33]. Our findings do not support obtaining routine barium radiography to confirm an IEM diagnosis. These radiographic studies were not timed barium swallows and the criteria for determining abnormal esophageal function on radiographic interpretation were not well codified. Radiographic studies that are performed following specific guidelines and interpretation may prove to correlate better, but they are likely only available at specialized centers.
Decreasing mean LES pressure was correlated with greater percent of ineffective contractions in both group 1 and all patients combined, with no correlation with failed contractions. In group 2, decreasing mean LES was associated with greater percent of failed contractions. There were similar significant findings between decreasing median IRP and increasing percent of ineffective or failed contractions among the groups. Significant findings between mean LES pressure and median IRP with motility findings on manometry may reflect an underlying smooth muscle pathology for IEM and warrant further study.
LES pressure is thought to contribute to the pathophysiology of GERD when LES pressure is lower than intragastric pressure. We did not find that GERD, reflux, and upper endoscopy finding of esophagitis were different between groups 1 and 2. Mean LES was also not associated with reflux or esophagitis. The high percentage of patients on PPI may minimize the findings of esophagitis in this study.
Symptoms and presentation of IEM have been described as gaps in the literature [2]. Dysphagia was the most common symptom included in the history or presentation for patients in both groups 1 and 2. The symptom of dysphagia was more prevalent in group 2, the group with less severe dysmotility. Dysphagia was not associated with liquid barium or barium tablet delay, incomplete bolus clearance, intrabolus pressure, nor percent of weak or failed contractions. These findings suggest that dysphagia is not primarily dependent on bolus transit in our study population. Similarly, Chugh et al (n = 33) found that patients with IEM, based on CCv3.0 criteria, and those with normal manometry studies did not differ in terms of symptom severity for dysphagia as defined by the Eckardt symptom score [33]. The researchers noted that a diagnosis of IEM was not helpful in assessing the degree of the symptom of dysphagia. The researchers did note an inverse correlation between dysphagia score and bolus clearance among IEM patients, which we were unable to replicate in our retrospective study due to lack of detailed dysphagia characteristics. The recent publication did not report a difference in Eckardt score between IEM patients defined by the CCv4.0 or CCv3.0 criteria [13].
A delay of liquid or solids during the oropharyngeal or esophageal phase of swallowing might lead to a person’s sensation of delay in transit which may be described as dysphagia. It is possible that some patients lose the sensation of delay in swallowing or have symptoms of delay due to sensory neural dysfunction. Dysphagia experienced by the patients meeting IEM CCv4.0 criteria could be due to a sensory or other component not analyzed in this study. It could also be due to somatization disorder given the high prevalence of depression and SSRI/SNRI usage among our study participants.
In analyzing the stability of manometric diagnoses among patients diagnosed with IEM, more patients diagnosed with IEM CCv4.0 maintained this diagnosis over time compared to patients diagnosed with IEM CCv3.0, although this finding was not statistically significant. The analysis was likely underpowered given the low number of patients who underwent more than one study. There was no association of time interval with stability of a manometric diagnosis. Triadafilopoulos et al examined repeat HRM studies based on CCv3.0 and determined that the fluidity in the HRM diagnosis over time raises questions concerning its validity at any timepoint and raises doubts about the need for intervention [34]. There have been no such studies analyzing repeat HRM studies based on CCv4.0.
There are several limitations to the study. It is a retrospective study that relies on existing information already captured in the medical record. Provocative studies such as multiple rapid swallows to examine contractile reserve, which are recommended in CCv4.0 manometric criteria for IEM, were not performed during the time of these studies. Multiple rapid swallow studies have been suggested to imply some motility abnormality in patients with symptoms or indeterminant findings, although there are no studies yet to support that hypothesis [35]. The value of this provocative study has been felt to be in predicting the risk of dysphagia after a fundoplication and the presence of contractile reserve in patients with absent peristalsis and is not critical to the diagnosis of IEM [36]. While it may be a useful adjunct to determining the severity of esophageal motor dysfunction, the classification of patients into our two diagnostic groups is not likely to have been changed by the addition of the provocative maneuver. The symptom of dysphagia was based on its inclusion in the medical record and was not assessed using a validated instrument; thus, severity and nuance of this symptom is not available. Analyses were not adjusted for by medication use since usage of those medications known to affect esophageal motility by group was not significantly different. The study was also limited to one hospital; therefore, findings about the patient population studied may not be generalizable to the entire IEM population. A control group was not utilized to study the prevalence of comorbidities and medication use among IEM patients to determine if these factors occur more frequently than among non-IEM patients.
In conclusion, in this review of 174 patients, a CCv4.0 IEM diagnosis was associated with worse esophageal function as indicated by incomplete bolus transit. This finding supports the CCv4.0 update for IEM as identifying more clinically significant cases and supports the value of obtaining a bolus impedance study when suspecting an IEM diagnosis. Many features studied did not differ between groups 1 and 2. Symptom of dysphagia was not associated with worse motility, suggesting that dysphagia may not be primarily dependent on bolus transit. Symptom presentation also cannot predict if patients are likely to have IEM by CCv4.0. The association of percent of ineffective contractions with lower mean LES pressure and median IRP suggests an underlying impaired contractile function. The impact on clinical outcome, and, possibly, further refinement of diagnostic criteria, needs further prospective study. This study builds on our understanding of the clinical and manometric characteristics of patients meeting IEM CCv4.0 criteria by evaluation of a larger patient group and examination of the associations between manometric features and with bolus clearance.
| Supplementary Material | ▴Top |
Suppl 1. Comorbidities by body system category.
Suppl 2. Association of the mean LES pressures among CCv4.0 IEM patients (n = 128), CCv3.0 only IEM patients (n = 46), or all patients combined (n = 174) with the presence of the symptom of dysphagia, reflux, or regurgitation or upper endoscopy finding of hiatal hernia or esophagitis, 2011 - 2019.
Suppl 3. Correlation of incomplete bolus clearance with median IRP among CCv3.0 IEM patients (n = 174), 2011 - 2019.
Suppl 4. Frequency of demographic and clinical characteristics among CCv4.0 IEM patients (n = 128) and CCv3.0 only IEM patients (n = 46), 2011 - 2019.
Suppl 5. Correlation of abnormal acid exposure (when esophageal pH is < 4 greater or equal to 4.2% of the time during the total study) with severity of weak contractions, severity of failed contractions, and mean LES pressure among CCv3.0 IEM patients not on PPI medication during pH impedance study (n = 17), 2011 - 2019.
Acknowledgments
We thank the Department of Medicine and Medical Student Research Program at the Penn State College of Medicine for supporting this project.
Financial Disclosure
Due to usage of REDCap, this project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR002014 and Grant UL1 TR00045. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Ann Ouyang was responsible for the conduct and oversight of this project. Alyssa Tuan, Nauroz Syed, Shannon Dalessio, Junjia Zhu, and Ann Ouyang were involved in study conception and design. Alyssa Tuan, Nauroz Syed, Ronaldo Panganiban, Roland Lee, Shannon Dalessio, Sandeep Pradhan, Junjia Zhu, and Ann Ouyang contributed to data analysis and interpretation. Alyssa Tuan, Ronaldo Panganiban, and Ann Ouyang contributed to manuscript preparation. All authors read and approved the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
BMI: body mass index; CCv3.0: Chicago Classification version 3.0; CCv4.0: Chicago Classification version 4.0; DCI: distal contractile integral; EGD: esophagogastroduodenoscopy; EGJOO: esophagogastric junction outlet obstruction; GERD: gastroesophageal reflux disease; HRM: high-resolution manometry; IEM: ineffective esophageal motility; IRB: Institutional Review Board; IRP: integrated relaxation pressure; LES: lower esophageal sphincter; NSAID: non-steroidal anti-inflammatory drug; PPI: proton pump inhibitor; SNRI: serotonin and norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor
| References | ▴Top |
- Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-174.
doi pubmed - Gyawali CP, Sifrim D, Carlson DA, Hawn M, Katzka DA, Pandolfino JE, Penagini R, et al. Ineffective esophageal motility: Concepts, future directions, and conclusions from the Stanford 2018 symposium. Neurogastroenterol Motil. 2019;31(9):e13584.
doi pubmed - Rogers BD, Rengarajan A, Mauro A, Ghisa M, De Bortoli N, Cicala M, Ribolsi M, et al. Fragmented and failed swallows on esophageal high-resolution manometry associate with abnormal reflux burden better than weak swallows. Neurogastroenterol Motil. 2020;32(2):e13736.
doi pubmed - Rengarajan A, Bolkhir A, Gor P, Wang D, Munigala S, Gyawali CP. Esophagogastric junction and esophageal body contraction metrics on high-resolution manometry predict esophageal acid burden. Neurogastroenterol Motil. 2018;30(5):e13267.
doi pubmed - Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33(1):e14058.
- Schlottmann F, Herbella FA, Patti MG. Understanding the Chicago Classification: From Tracings to Patients. J Neurogastroenterol Motil. 2017;23(4):487-494.
doi pubmed - Shi Z, Guo J, Clarke J, Jin H, Wang X, Zhang N, Stein E, et al. Roles of high-resolution manometry in predicting incomplete bolus transit in patients with dysphagia. J Clin Gastroenterol. 2018;52(9):e73-e81.
doi pubmed - Jain A, Baker JR, Chen JW. In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil. 2018;30(6):e13297.
doi pubmed - Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
doi pubmed - Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
doi pubmed - SAS Institute. 2015. SAS 9.4 macro language: Reference.
- Zhuang QJ, Tan ND, Zhang MY, Chen SF, Luo Y, Xiao YL. Ineffective esophageal motility in Chicago Classification version 4.0 better predicts abnormal acid exposure. Esophagus. 2022;19(1):197-203.
doi pubmed - Sallette M, Lenz J, Mion F, Roman S. From Chicago classification v3.0 to v4.0: Diagnostic changes and clinical implications. Neurogastroenterol Motil. 2023;35(1):e14467.
doi pubmed - Centers for Disease Control and Prevention. Adult Obesity Facts. June 7, 2021. Accessed on August 22, 2021.
- Shetler KP, Bikhtii S, Triadafilopoulos G. Ineffective esophageal motility: clinical, manometric, and outcome characteristics in patients with and without abnormal esophageal acid exposure. Dis Esophagus. 2017;30(6):1-8.
doi pubmed - Pakoz ZB, Sari SO, Vatansever S, Uran BNO, Camyar H, Gur EO, Gumus ZZ, et al. Ineffective esophageal motility assessment in patients with and without pathological esophageal acid reflux. Medicine (Baltimore). 2021;100(20):e26054.
doi pubmed - Nikaki K, Sawada A, Ustaoglu A, Sifrim D. Neuronal Control of Esophageal Peristalsis and Its Role in Esophageal Disease. Curr Gastroenterol Rep. 2019;21(11):59.
doi pubmed - Choi JM, Yang JI, Kang SJ, Han YM, Lee J, Lee C, Chung SJ, et al. Association between anxiety and depression and gastroesophageal reflux disease: results from a large cross-sectional study. J Neurogastroenterol Motil. 2018;24(4):593-602.
doi pubmed - On ZX, Grant J, Shi Z, Taylor AW, Wittert GA, Tully PJ, Hayley AC, et al. The association between gastroesophageal reflux disease with sleep quality, depression, and anxiety in a cohort study of Australian men. J Gastroenterol Hepatol. 2017;32(6):1170-1177.
doi pubmed - Moosavi S, Woo M, Jacob DA, Pradhan S, Wilsack L, Buresi M, Gupta M, et al. Anticholinergic, anti-depressant and other medication use is associated with clinically relevant oesophageal manometric abnormalities. Aliment Pharmacol Ther. 2020;51(11):1130-1138.
doi pubmed - Mikami DJ, Murayama KM. Physiology and pathogenesis of gastroesophageal reflux disease. Surg Clin North Am. 2015;95(3):515-525.
doi pubmed - Wong MW, Hung JS, Lei WY, Yi CH, Liu TT, Chen CL. Influence of sildenafil on esophageal motor function in humans: Studies using high-resolution manometry. Neurogastroenterol Motil. 2020;32(7):e13840.
doi pubmed - Rangan V, George NS, Khan F, Geng Z, Gabbard S, Kichler A, Gittleman H, et al. Severity of ineffective esophageal motility is associated with utilization of skeletal muscle relaxant medications. Neurogastroenterol Motil. 2018;30(4):e13235.
doi pubmed - Ratuapli SK, Crowell MD, DiBaise JK, Vela MF, Ramirez FC, Burdick GE, Lacy BE, et al. Opioid-Induced Esophageal Dysfunction (OIED) in patients on chronic opioids. Am J Gastroenterol. 2015;110(7):979-984.
doi pubmed - Babaei A, Szabo A, Shad S, Massey BT. Chronic daily opioid exposure is associated with dysphagia, esophageal outflow obstruction, and disordered peristalsis. Neurogastroenterol Motil. 2019;31(7):e13601.
doi pubmed - Achem SR, Kolts BE. Current medical therapy for esophageal motility disorders. Am J Med. 1992;92(5A):98S-105S.
doi pubmed - Patel DA, Yadlapati R, Vaezi MF. Esophageal motility disorders: current approach to diagnostics and therapeutics. Gastroenterology. 2022;162(6):1617-1634.
doi pubmed - Philpott HL, Nandurkar S, Lubel J, Gibson PR. Drug-induced gastrointestinal disorders. Postgrad Med J. 2014;90(1065):411-419.
doi pubmed - Sopena F, Lanas A, Sainz R. Esophageal motility and intraesophageal pH patterns in patients with esophagitis and chronic nonsteroidal anti-inflammatory drug use. J Clin Gastroenterol. 1998;27(4):316-320.
doi pubmed - Richter JE. Chicago Classification Version 4.0 and its impact on current clinical practice. Gastroenterol Hepatol (N Y). 2021;17(10):468-475.
- Triadafilopoulos G, Tandon A, Shetler KP, Clarke J. Clinical and pH study characteristics in reflux patients with and without ineffective oesophageal motility (IEM). BMJ Open Gastroenterol. 2016;3(1):e000126.
doi pubmed - Zerbib F, Marin I, Cisternas D, Abrahao L, Jr., Hani A, Leguizamo AM, Remes-Troche JM, et al. Ineffective esophageal motility and bolus clearance. A study with combined high-resolution manometry and impedance in asymptomatic controls and patients. Neurogastroenterol Motil. 2020;32(9):e13876.
doi pubmed - Chugh P, Collazo T, Dworkin B, Jodorkovsky D. Ineffective esophageal motility is associated with impaired bolus clearance but does not correlate with severity of dysphagia. Dig Dis Sci. 2019;64(3):811-814.
doi pubmed - Triadafilopoulos G, Kamal A, Zikos T, Nguyen L, Clarke JO. Changes in high-resolution manometric diagnosis over time: implications for clinical decision-making. Dis Esophagus. 2020;33(3):doz094.
doi pubmed - Leopold A, Yu D, Bhuta R, Kataria R, Lu X, Jehangir A, Harrison M, et al. Multiple Rapid Swallows (MRS) Complements Single-Swallow (SS) Analysis for High-Resolution Esophageal Manometry (HREM). Dig Dis Sci. 2019;64(8):2206-2213.
doi pubmed - Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108(11):1706-1712.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


