| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Case Report
Volume 15, Number 3, June 2022, pages 142-147
Upper Gastrointestinal Cancer: Delays in Diagnosis and Treatment Caused by Barriers to Healthcare in the Latino Community
Eleazar E. Montalvan-Sancheza, f , Renato Beasa
, Dalton Argean Norwoodb
, Ahmad Mahmoud Alkashashc
, Aida A. Rodriguez Murillod, e, Gerardo Calderona
aDepartment of Medicine, Indiana University School of Medicine, Indianapolis, IN 46202, USA
bDivision of Preventive Medicine, University of Alabama at Birmingham, Birmingham, AL 35294, USA
cDepartment of Pathology, Indiana University School of Medicine, Indianapolis, IN 46202, USA
dWestern Honduras Gastric Cancer Prevention Initiative, Hospital de Occidente, Santa Rosa de Copan, Honduras
eUniversidad Nacional Autonoma de Honduras, School of Medicine, Tegucigalpa, Honduras
fCorresponding Author: Eleazar E. Montalvan-Sanchez, Department of Medicine, Indiana University School of Medicine, Indianapolis, IN 46202, USA
Manuscript submitted February 28, 2022, accepted April 7, 2022, published online June 16, 2022
Short title: GI Cancer Disparities in Latino Community
doi: https://doi.org/10.14740/gr1514
| Abstract | ▴Top |
We report a case of an 81-year-old male immigrant from a Latin American developing country with a high burden of upper gastrointestinal neoplasms, who presented with a small bowel gastrointestinal stromal tumor (GIST) after 2 years of delay in the diagnosis due to multiple barriers to healthcare. The patient presented with a partial intestinal obstruction in an abdominal computed tomography (CT) scan suggestive of a GIST. Surgical resection was performed, and adjuvant therapy was initiated with imatinib (a tyrosine kinase inhibitor) after the diagnosis was confirmed. The patient had a successful outcome. Due to his migratory status, the patient planned to follow up with different health providers in two different countries, which constitutes a common challenge in the immigrant population.
Keywords: GIST; Upper gastrointestinal tract; Hispanic or Latino; Healthcare disparities; Health services accessibility
| Introduction | ▴Top |
The overall cancer incidence in Latin America has increased, with mortality rates being higher when compared to developed countries mainly due to decreased underfunded healthcare systems which are often difficult to access [1, 2]. Health care access remains an important public health issue, especially in rural areas in Latin America, which are related to geographical locations, transportation limitations, and health costs [3-5].
There is scarce literature reporting the incidence of gastrointestinal stromal tumors (GISTs) in Latin America in contrast to North American, European, and Asian populations. A systematic review by Calderillo et al reported an incidence of 9.7 cases of GIST per million in Mexican and Chilean populations with high incidence in the stomach and small intestine [6]. GIST involvement of the upper gastrointestinal tract has been frequently described among the Latino population in the USA and has been associated with a higher metastatic rate at the time of diagnosis and poor prognosis [7]. Approximately 25% of patients with upper gastrointestinal neoplasms present with no alarm symptoms and have an insidious progression with limited survival benefit achieved if not detected early [8, 9]. There is a lack of case reports and population-based perspectives of GIST prevalence and incidence in the Hispanic population living in the USA.
Surgical resection remains the cornerstone for localized GIST, with endoscopic procedures offering the option of resection on early stages [10, 11]. Imatinib, a tyrosine kinase inhibitor (TKI), has improved outcomes when used as preoperative and adjuvant treatment [11, 12]. Developing countries, such as Honduras, usually suffer a lack of effective diagnostic and treatment capacity for gastrointestinal neoplasms, therefore the prognosis is very poor. We report a case of an 81-year-old Honduran male with poor social support, who presented with partial small bowel obstruction secondary to a large GIST in the small intestine after delays in diagnosis and treatment due to healthcare barriers.
| Case Report | ▴Top |
Investigations
An 81-year-old Hispanic male from Honduras with 2-year history of abdominal mass without previous workup due to limited resources, Helicobacter pylori (H. pylori) status post eradication, and no established medical care in the USA presented to the emergency department with acute severe abdominal vomiting and an absence of bowel movements for 2 days. On the day of admission, physical examination showed severe abdominal distention and a palpable mass localized in the right upper quadrant of the abdomen with a smooth surface and edges of hard consistency. Also, the patient was found with a body mass index (BMI) of 19. Laboratory studies on admission only revealed marked hypoalbuminemia. Complete blood count, comprehensive metabolic panel, electrolytes, and infectious workup were found within normal limits.
Diagnosis
An abdomen and pelvis computed tomography (CT) scan with contrast was performed and revealed an intraabdominal mass arising from the upper gastrointestinal tract and measuring 11 × 14 × 10 cm (Fig. 1). While hospitalized, a plan for surgery was made due to worsening abdominal pain and partial small bowel obstruction secondary to a possible malignancy. The patient’s poor nutritional state foreshadowed a high risk of complications. In that sense, a 3-week program of nutritional optimization before surgery was planned. A high-energy, high-protein diet was instituted with total parenteral nutrition and daily physiotherapy. During his hospital stay, a series of multidisciplinary meetings were held to help with the patient’s goals of care. There was uncertainty due to cultural and language barriers in the conversations and previous lack of medical care.
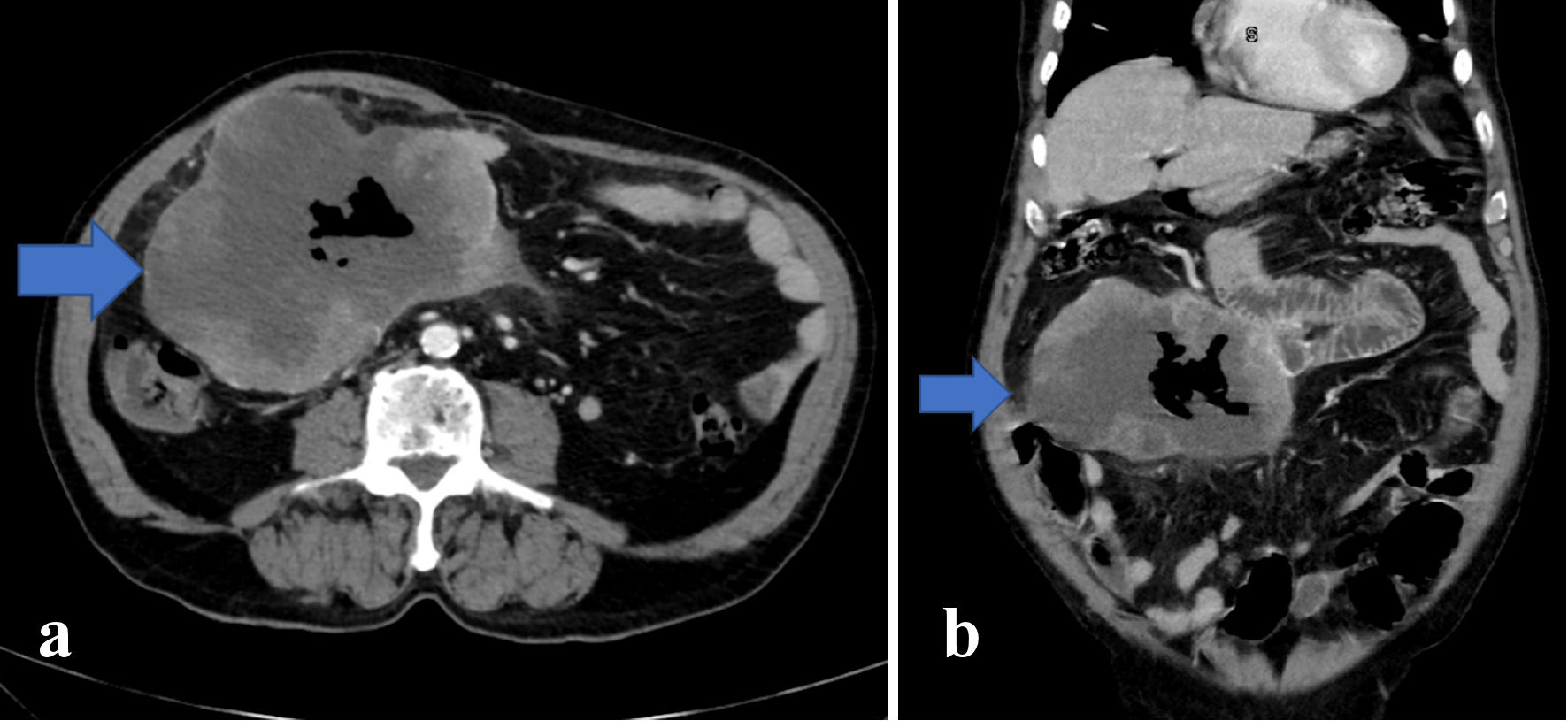 Click for large image | Figure 1. Axial (a) and coronal (b) images of abdominal CT scan indicate a sizeable mass (arrow) adjacent to the proximal duodenum with central necrosis and gas-containing, measuring approximately 11 × 14 × 10 cm. Also, distention of the bowels right adjacent to the mass is noticeable without proximal distension. CT: computed tomography. |
Treatment
The progression of the patient’s symptoms precluded a more extended rehabilitation period, and by the third week of nutritional support and physiotherapy, a surgical procedure was performed. A midline laparotomy exposed a 30 cm mass coming from the small bowel, and dissection allowed the separation of the mass from the small bowel in two locations. Both of these areas were resected with subsequent reanastomosis. The tissue sample obtained was positive for a malignant neoplasm with spindle cell morphology, tumor necrosis, and occasional mitoses. Tumor cells were positive for c-kit/CD117 marker and DOG1 (Discovered on GIST 1) with a mitotic rate of 2/5 mm2, confirming GIST diagnosis (Fig. 2).
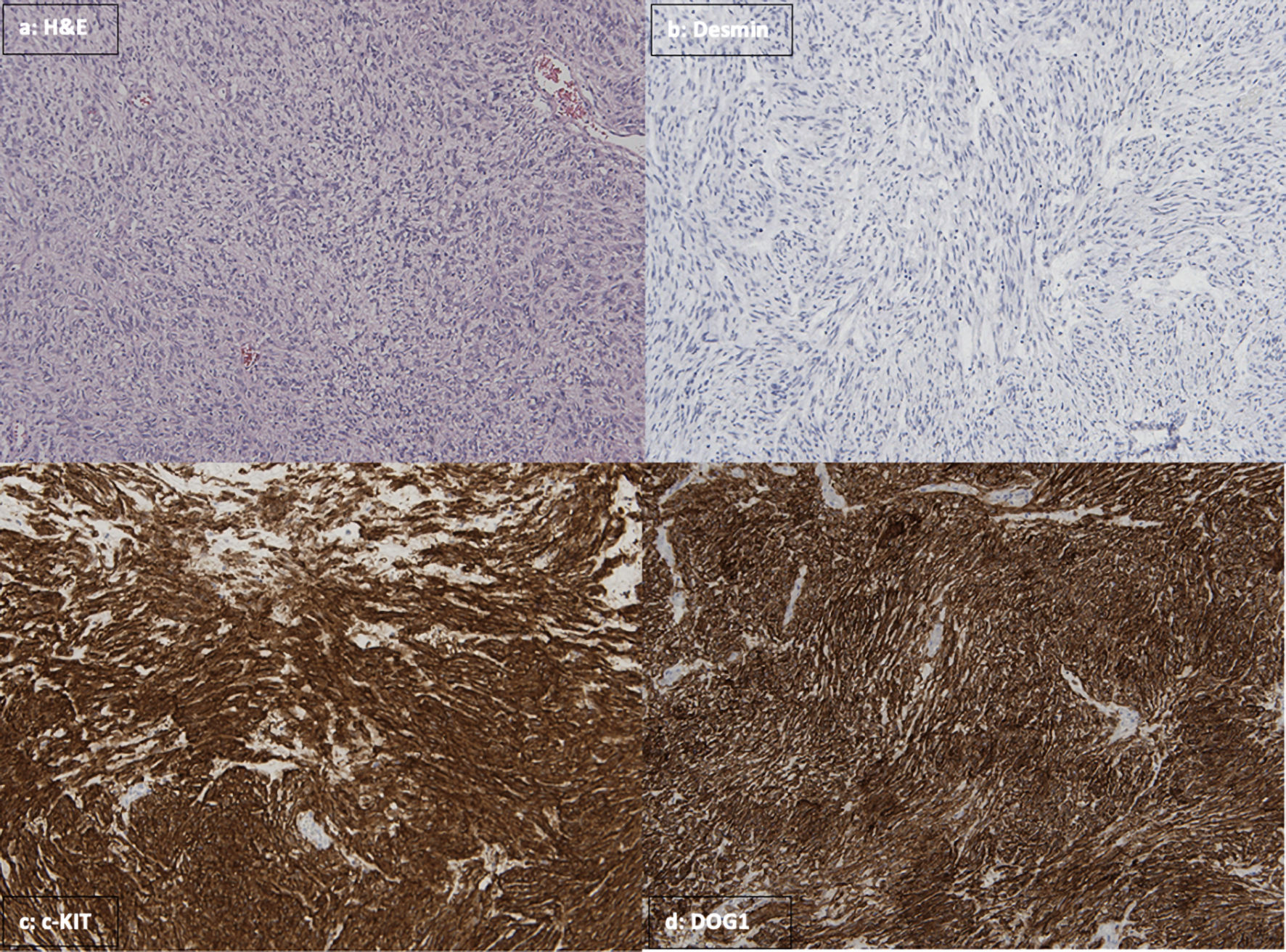 Click for large image | Figure 2. (a) In H&E stain, sections from the lesion showing the tumor spindle cell morphology and occasional mitoses. Immunohistochemical stains were performed, showing the tumor cells are negative for desmin (b), while strongly positive for c-kit/CD117 (c) and DOG1 (d). H&E: hematoxylin and eosin; DOG1: Discovered on GIST 1. |
Follow-up and outcomes
A chest CT was also obtained and showed no evidence of metastasis. Genetic testing revealed a KIT gene exon 11 with no mutations in the PDGFRA genes. The patient recovered well from the postoperative period, and after an oncology evaluation and a multidisciplinary meeting, imatinib was added for adjuvant therapy. A 4-week follow-up with positron emission tomography (PET) scan was negative for focal uptake of fluorodeoxyglucose with no increased uptake suspicious for metastasis or residual disease. The patient was discharged with recommendations of continuing care and scheduled follow-up with general surgery, oncology, gastroenterology, and palliative care providers. However, the patient decided to return to his home country where he would establish care with a new primary provider.
| Discussion | ▴Top |
The Hispanic population is the fastest growing ethnic group in the USA, becoming the largest minority group (18%, 48 million) and expected to account for one quarter of the USA population by 2050 [13, 14]. Health disparities have been widely studied in the Latino population, identifying several social determinants of health (SDOH), such as health coverage, provider linguistic, cultural competency, economic stability, and education, leading to non-established health status and consequent underdiagnosis of chronic diseases such as cancer [7, 15]. Several studies had described the hesitancy among minorities to perform cancer screenings or cancer prevention strategies [16, 17].
This case report exhibits multiple barriers to healthcare that were identified during the patient’s prolonged disease course. First, healthcare access is difficult due to hometown being located in a mountainous region of Honduras distant to secondary or tertiary healthcare centers, despite being a known region with a high incidence of upper gastrointestinal neoplasm [18-20]. Additionally, in low-middle-income countries, the recommended radiological and endoscopic studies for detecting these intraabdominal conditions are not available in many hospitals and, when available, are expensive, contributing to the delay of diagnosis and treatment [19, 21].
Barriers to healthcare were not only limited to the patient’s country of origin only. During his stay in the USA, the patient’s lack of health insurance due to migratory status, being a non-English speaker, and fear of being discriminated during the first health care contact led him and his family to avoid visiting the emergency department early in the disease course. These obstacles usually found by the Latino community impact negatively in health outcomes, such as lack of cancer screenings for age and sex, a late diagnosis such as malignancies at late stages, and further increasing the mortality. The aforementioned barriers further increase the health inequities among this population when compared to non-Hispanic whites [22-24] (Fig. 3).
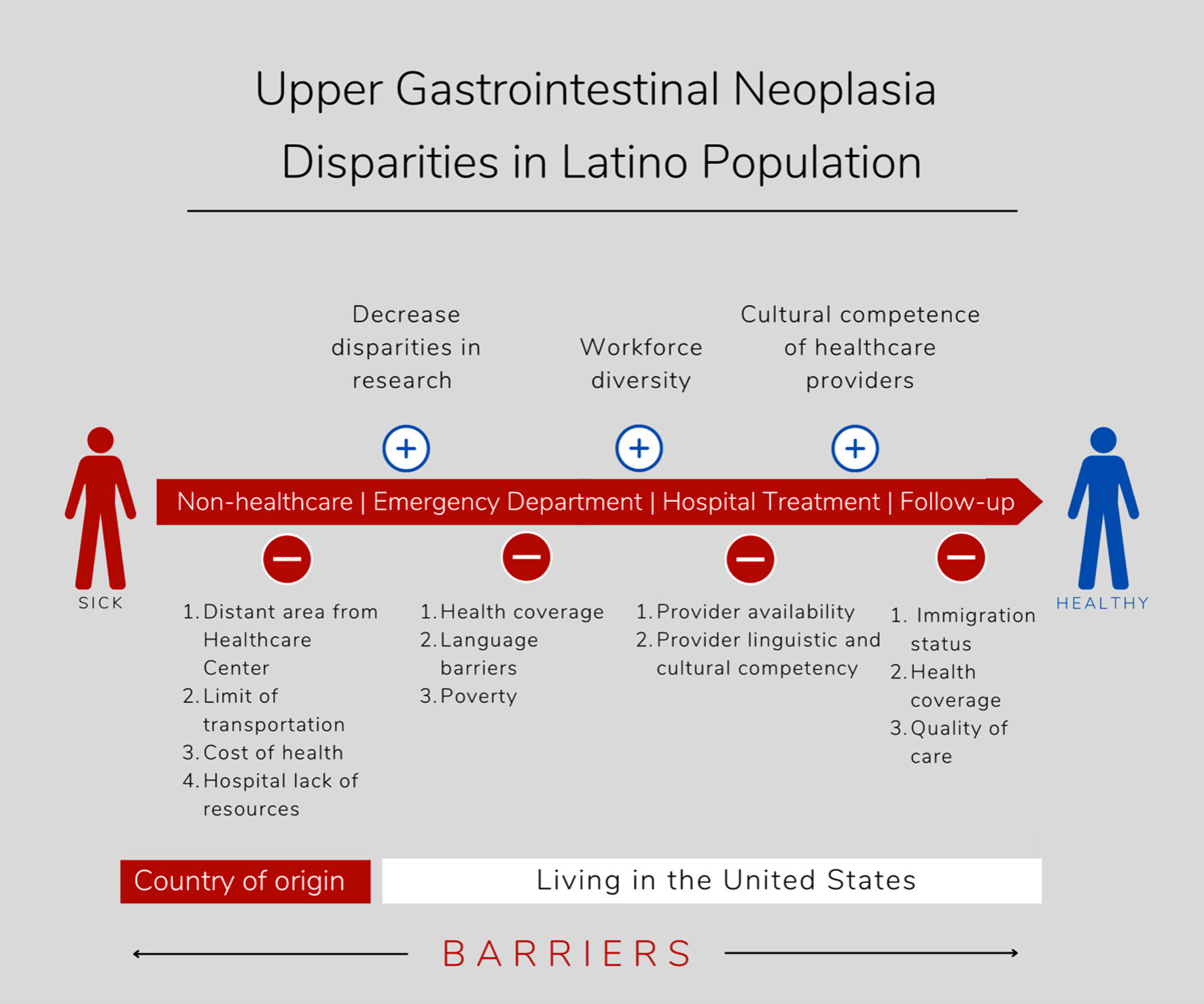 Click for large image | Figure 3. Barriers to access to health care encountered by the Latino population in their countries of origin and moving to the USA, including barriers to visit the emergency department, during hospitalization for treatment, and outpatient specialty clinic follow-up. |
It is known that upper gastrointestinal neoplasms are the leading cause of malignancies and mortality in Central America, and impact the USA health system as Central America forms the second largest Latino immigrant population [18-21, 25].
The lack of access to healthcare makes it difficult to assess the real burden of GIST in the Latino population. The annual incidence of GIST in the USA is at least 3,330 - 6,000 new GIST cases per year, with 6.8 cases per million population [26, 27]. As the most common mesenchymal tumor of the gastrointestinal tract, the most frequent anatomical location of GIST is gastric (55.6%), followed by small bowel (31.8%), and colorectal (6.0%) [26, 27].
The initial evaluation and assessment of GIST require imaging modalities that support the diagnosis. The contrast-enhanced CT scan is the standard method for GIST imaging [28]. However, diagnosis is challenging given other potential mimicking conditions such as intestinal tuberculosis, amebomas, or lymphomas that could simulate and are also prevalent in Latin-American countries.
The gold standard of treatment for GIST is the laparoscopic/open excision approach. With the widespread of endoscopic ultrasound, more early stages of GIST are diagnosed. The advances of endoscopically submucosal dissections also provide part of management for upper gastrointestinal GIST [29].
GIST clinical presentation and course can vary depending on every case. In the case presented, our patient had mild epigastric pain and dyspepsia with a prodrome of vague symptoms for over 2 years, characteristics of upper gastrointestinal neoplasms [30, 31]. Patients usually present with gastrointestinal bleeding, obstruction, abdominal pain, or even incidental findings during imaging or other surgeries [32]. Our patient presented with an acute partial intestinal obstruction due to the mass effect of the tumor by its size.
This patient’s clinical presentation is typical of an advanced upper gastrointestinal neoplasm with late manifestations and increased mortality [18]. The prognosis is significantly worse, and the local implications for surgery tend to be more critical [26, 27]. After goals of care discussion during family meetings with a multidisciplinary team with palliative care, oncology, gastroenterology, and surgery, finally the patient was successfully taken to the operative room.
It is essential to recognize that Latino elders, as our patient, have significant barriers to health literacy. Considering most immigrants are from rural areas with a language barrier, different health and religious beliefs, this topic should be considered as part of discussing goals of care and surgical procedures. Like what our patient requested for, most of them prefer to have a family as a decision-maker. They usually avoid aggressive treatments, and the advanced directives are not usually previously discussed with the family or health care providers. Having healthcare providers from a similar ethnic background and speaking Spanish was essential to provide high quality care [33, 34]. The authors encourage whenever possible to involve an interdisciplinary team with a Latino health provider being part of these conversations.
In the follow-up clinic, the pathology result was positive for tumor cells with c-kit/CD117. Adjuvant treatment was started with imatinib with a plan of a 3-year course that is associated with relapse-free survival and overall survival compared to 1-year course in a high-risk patient. This diagnosis with c-kit/CD117 markers and treatment with TKI are not globally accessible. For our patient, this mechanism of diagnosis or adjuvant treatment will not be possible in his home country.
The patient had to return to his home country due to his migratory status with a tentative plan to return to the USA in 6 months. Follow-up laboratory studies were recommended. His family planned to send imatinib as this medication was unavailable in his home country.
With the constant informal immigration from these countries to the USA, surveillances for upper gastrointestinal neoplasms and policies for prevention in this high-risk population should be established. Health systems should provide an adequate bilingual health workforce to maximize health care quality. Access to health is one of the fundamental rights of every human being. The delay of diagnosis and treatment in our patient demonstrates the lack of access to health in rural Honduras and the immigrant population in the USA.
Learning points
Access to health care is a significant public health issue, especially in rural areas related to geographical locations, limits of transportation, and health costs.
Latino immigrants struggle to receive medical care in the USA due to a lack of health insurance economic and language barriers.
Hispanic populations present an increased risk of upper gastrointestinal neoplasm compared to non-Hispanic whites.
Upper gastrointestinal neoplasms are the leading cause of mortality secondary to malignancies in Central America.
The lack of access to healthcare makes it difficult to assess the real burden of GIST disease in Latin America.
Acknowledgments
We acknowledge the following individual, Mirian Ramirez from Ruth Lily Medical Library, for the support and literature review provided to the Latino gastroenterology research group in Indiana University School of Medicine.
Financial Disclosure
None to declare.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Informed consent was provided by the patient.
Author Contributions
EEMS, GC, and RB are the leading role in patient care and diagnosis. EEMS, RB, DAN, AMA, AARM and GC executed the study literature review. AMA analyzed the pathology samples. All authors provided the overall data interpretation and oversight. All authors provided a critical review of the manuscript and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
GIST: gastrointestinal stromal tumor; TKI: tyrosine kinase inhibitor; SDOH: social determinants of health; PET: positron emission tomography
| References | ▴Top |
- Goss PE, Lee BL, Badovinac-Crnjevic T, Strasser-Weippl K, Chavarri-Guerra Y, St Louis J, Villarreal-Garza C, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. 2013;14(5):391-436.
doi - Ruiz R, Strasser-Weippl K, Touya D, Herrero Vincent C, Hernandez-Blanquisett A, St Louis J, Bukowski A, et al. Improving access to high-cost cancer drugs in Latin America: Much to be done. Cancer. 2017;123(8):1313-1323.
doi pubmed - Maria Leonor Maia KL, Geraldo Marinho, Enilson Santos, Jessica Helena de Lima. Access to the Brazilian City - from the perspectives of low-income residents in Recife. Journal of Transport Geography. 2016;55:132-141.
doi - Garcia E, Serban N, Swann J, Fitzpatrick A. The effect of geographic access on severe health outcomes for pediatric asthma. J Allergy Clin Immunol. 2015;136(3):610-618.
doi pubmed - Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, Hudson M. What does 'access to health care' mean? J Health Serv Res Policy. 2002;7(3):186-188.
doi pubmed - Calderillo G, Munoz-Medel M, Carbajal E, Cordova-Delgado M, Duran D, Retamal IN, Fernandez P, et al. Retrospective Analysis of Chilean and Mexican GI Stromal Tumor Registries: A Tale of Two Latin American Realities. JCO Glob Oncol. 2020;6:647-657.
doi pubmed - Ulanja MB, Rishi M, Beutler BD, Konam KG, Ambika S, Hinojosa T, Djankpa FT, et al. Racial Disparity in Incidence and Survival for Gastrointestinal Stromal Tumors (GISTs): an Analysis of SEER Database. J Racial Ethn Health Disparities. 2019;6(5):1035-1043.
doi pubmed - Rasmussen S, Haastrup PF, Balasubramaniam K, Christensen RD, Sondergaard J, Jarbol DE. Predictive values of upper gastrointestinal cancer alarm symptoms in the general population: a nationwide cohort study. BMC Cancer. 2018;18(1):440.
doi pubmed - Fransen GA, Janssen MJ, Muris JW, Laheij RJ, Jansen JB. Meta-analysis: the diagnostic value of alarm symptoms for upper gastrointestinal malignancy. Aliment Pharmacol Ther. 2004;20(10):1045-1052.
doi pubmed - Tan Y, Tan L, Lu J, Huo J, Liu D. Endoscopic resection of gastric gastrointestinal stromal tumors. Transl Gastroenterol Hepatol. 2017;2:115.
doi pubmed - Casali PG, Blay JY, Abecassis N, Bajpai J, Bauer S, Biagini R, Bielack S, et al. Gastrointestinal stromal tumours: ESMO-EURACAN-GENTURIS clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022;33(1):20-33.
doi pubmed - Reichardt P. The Story of Imatinib in GIST - a Journey through the Development of a Targeted Therapy. Oncol Res Treat. 2018;41(7-8):472-477.
doi pubmed - Passel JS, Cohn D, Lopez MH. Census 2010: 50 million latinos. Hispanics account for more than half of the Nation's growth in past decade. Washington, DC: Pew Research. 2011.
- Colby S, Ortman JM. Projections of the size and composition of the US population: 2014 to 2060. 2015.
- Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, Davis D, Escamilla-Cejudo JA. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;37:31.
doi pubmed - Brandzel S, Chang E, Tuzzio L, Campbell C, Coronado N, Bowles EJ, Bradford SC, et al. Latina and Black/African American women's perspectives on cancer screening and cancer screening reminders. J Racial Ethn Health Disparities. 2017;4:1000-1008.
doi pubmed - Khodadadi AB, Redden DT, Scarinci IC. HPV vaccination hesitancy among latina immigrant mothers despite physician recommendation. Ethn Dis. 2020;30(4):661-670.
doi pubmed - Estevez-Ordonez D, Montalvan-Sanchez EE, Wong RE, Montalvan-Sanchez DM, Rodriguez-Murillo AA, Dominguez RL, Morgan DR. Health barriers and patterns of gastric cancer care in rural central American resource-limited settings. JAMA Oncol. 2018;4(8):1131-1133.
doi pubmed - Norwood DA, Montalvan-Sanchez EE, Corral JE, Estevez-Ordonez D, Paredes AA, Dominguez LB, Rodriguez AA, et al. Western Honduras Copan population-based cancer registry: initial estimates and a model for rural central America. JCO Glob Oncol. 2021;7:1694-1702.
doi pubmed - Torres J, Correa P, Ferreccio C, Hernandez-Suarez G, Herrero R, Cavazza-Porro M, Dominguez R, et al. Gastric cancer incidence and mortality is associated with altitude in the mountainous regions of Pacific Latin America. Cancer Causes Control. 2013;24(2):249-256.
doi pubmed - Rawla P, Barsouk A. Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol. 2019;14(1):26-38.
doi pubmed - Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. 2013;20(2):155-161.
doi pubmed - Fleming PJ, Novak NL, Lopez WD. U.S. Immigration Law Enforcement Practices and Health Inequities. Am J Prev Med. 2019;57(6):858-861.
doi pubmed - Morgan DR, Rojas C, Prata EM, Cohen MG, Ferris M, Rivadeneira AC, Kizer JS, et al. Novel academic center model for Spanish-speaking patients in the southeastern United States. Prev Med Community Health. 2020;3(1):1-7.
doi - Corral JE, Delgado Hurtado JJ, Dominguez RL, Valdez de Cuellar M, Balmore Cruz C, Morgan DR. The descriptive epidemiology of gastric cancer in Central America and comparison with United States Hispanic populations. J Gastrointest Cancer. 2015;46(1):21-28.
doi pubmed - Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100(1):162-168.
doi pubmed - Corless CL, Ballman KV, Antonescu CR, Kolesnikova V, Maki RG, Pisters PW, Blackstein ME, et al. Pathologic and molecular features correlate with long-term outcome after adjuvant therapy of resected primary GI stromal tumor: the ACOSOG Z9001 trial. J Clin Oncol. 2014;32(15):1563-1570.
doi pubmed - Kalkmann J, Zeile M, Antoch G, Berger F, Diederich S, Dinter D, Fink C, et al. Consensus report on the radiological management of patients with gastrointestinal stromal tumours (GIST): recommendations of the German GIST Imaging Working Group. Cancer Imaging. 2012;12:126-135.
doi pubmed - Tan M, Lahiff C, Bassett P, Bailey AA, East JE. Efficacy of balloon overtube-assisted colonoscopy in patients with incomplete or previous difficult colonoscopies: a meta-analysis. Clin Gastroenterol Hepatol. 2017;15(10):1628-1630.
doi pubmed - Soreide K, Sandvik OM, Soreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39-46.
doi pubmed - Craanen ME, Dekker W, Ferwerda J, Blok P, Tytgat GN. Early gastric cancer: a clinicopathologic study. J Clin Gastroenterol. 1991;13(3):274-283.
doi pubmed - Eisenberg BL, Pipas JM. Gastrointestinal stromal tumor—background, pathology, treatment. Hematol Oncol Clin North Am. 2012;26(6):1239-1259.
doi pubmed - Cruz-Oliver DM, Talamantes M, Sanchez-Reilly S. What evidence is available on end-of-life (EOL) care and Latino elders? A literature review. Am J Hosp Palliat Care. 2014;31(1):87-97.
doi pubmed - Fischer SM, Sauaia A, Min SJ, Kutner J. Advance directive discussions: lost in translation or lost opportunities? J Palliat Med. 2012;15(1):86-92.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


