| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Case Report
Volume 12, Number 2, April 2019, pages 96-99
Thrombocytosis as a Rare Paraneoplastic Syndrome Occurring in Hepatocellular Carcinoma: A Case Report
Hafsa Abbasa, c, Sana Hanifb, Hassan Tariqa, Sridhar Chilimurib
aDivision of Gastroenterology, Department of Medicine, Bronxcare Hospital Center, Bronx, NY 10457, USA
bDepartment of Medicine, Bronxcare Hospital Center, Bronx, NY 10457, USA
cCorresponding Author: Hafsa Abbas, Division of Gastroenterology, Department of Medicine, Bronxcare Hospital Center, Bronx, NY 10457, USA
Manuscript submitted January 27, 2019, accepted February 21, 2019
Short title: Thrombocytosis Occurring in HCC
doi: https://doi.org/10.14740/gr1137
| Abstract | ▴Top |
Hepatocellular carcinoma (HCC) affects more than half a million people worldwide each year. Paraneoplastic syndromes associated with HCC include erythrocytosis, hypercalcemia, hypercholesterolemia, hypoglycemia and thrombocytosis. Thrombocytosis is a rare paraneoplastic syndrome in HCC mediated by thrombopoietin (TPO) production. We report a case of thrombocytosis as a paraneoplastic syndrome in a patient with HCC and hepatitis C cirrhosis. A 56-year-old patient was evaluated with abdominal distension and pain of 1-month duration. He had a history of hepatitis C infection with liver cirrhosis, CTP (Child-Turcotte-Pugh) class C, MELD (model for end-stage liver disease) score 22, methadone dependence, alcohol abuse and depression. His physical examination was remarkable for distended abdomen with shifting dullness, palpable hepatomegaly and scleral icterus. Routine laboratory tests showed a platelet count of 754 k/µL, white blood cell count 12.4 k/µL, serum sodium level 128 mEq/L, alanine aminotransferase 93 U/L, aspartate aminotransferase 871 U/L, total serum bilirubin 4.3 mg/dL, direct serum bilirubin 2.8mg/dL and albumin 2.6 g/dL. Computed tomography of the abdomen and pelvis revealed hepatomegaly with numerous hypodensities suspicious for HCC. Abdominal paracentesis was done, serum ascites albumin gradient (SAAG) was 2.4 g/dL consistent with portal hypertension, and spontaneous bacterial peritonitis was ruled out. Magnetic resonance imaging of the liver was consistent with infiltrating HCC, portal vein thrombosis and retroperitoneal lymphadenopathy. His alpha fetoprotein (AFP) level was 79,102 ng/mL and TPO level was 126 pg/mL. JAK2 mutation was negative and no other cause of reactive thrombocytosis could be identified. One year prior to this admission, the patient was noted to have a normal platelet count and AFP level. He was not considered a candidate for liver transplantation due to ongoing substance abuse, and expired 1 month later. Thrombocytosis is a rare paraneoplastic condition seen in HCC. It is presumed to be secondary to increased production of TPO by the tumor. We observed an elevated level of TPO in our patient. Thrombocytosis in HCC is associated with a high tumor burden, portal vein thrombosis (PVT), serum AFP levels and a poor prognosis. Thrombocytosis in a cirrhotic patient should alert the presence of HCC and is associated with poor outcomes.
Keywords: Hepatocellular carcinoma; Paraneoplastic syndrome; Thrombocytosis
| Introduction | ▴Top |
Hepatocellular carcinoma (HCC) is seen in more than half a million people worldwide each year with approximately 20,000 new cases in United States [1, 2]. It is the fifth most common malignancy in men and seventh most common malignancy in women. In the developing world, it is seen in association with hepatitis B virus infection. In the United States the incidence of HCC is on the rise and is seen increasingly in association with hepatitis C virus infection [3].
Thrombocytopenia has been reported as a risk factor and as a prognostic indicator for HCC [4], however, thrombocytosis is rare. There are a variety of paraneoplastic syndromes associated with HCC including erythrocytosis, hypercalcemia, hypercholesterolemia, hypoglycemia and Thrombocytosis [5]. Thrombocytosis is a rare paraneoplastic syndrome in HCC and is thought to be mediated by thrombopoietin (TPO) production.
Few cases have been reported in medical literature of thrombocytosis coexisting with HCC. We report a case of thrombocytosis as a paraneoplastic syndrome in a patient with HCC and hepatitis C cirrhosis.
| Case Report | ▴Top |
A 56-year-old man was evaluated in the emergency room of our hospital with abdominal pain, abdominal distension and bilateral leg swelling of 1-month duration. The patient reported that his symptoms started 1 month ago and had been progressively getting worse over the week prior to index presentation. He described the abdominal pain as constant, diffuse, non-radiating and moderate in intensity without any precipitating or relieving factors. He reported one episode of diarrhea which did not contain any blood. There was no nausea, vomiting, constipation, fever, and early satiety or appetite changes. He had a history of hepatitis C infection with cirrhosis of the liver, Child-Turcotte-Pugh (CTP) class C, model for end-stage liver disease (MELD) score 22, methadone dependence, alcohol abuse and depression. Patient was a former smoker, had a history of substance abuse and was enrolled in a methadone program. He did not have a family history of liver or colon cancer. His medications included albuterol, folic acid, multi-vitamins, thiamine, citalopram and methadone.
On examination, he was found to have temperature of 36.8 °C, blood pressure of 138/84 mm Hg, pulse rate of 93 beats per minute and the respiratory rate of 14 breaths per minute. The patient was noted to have scleral icterus along with yellowish discoloration of the skin, spider angiomata on the upper chest, head and upper extremities. The abdomen was distended, diffusely tender with a positive fluid thrill and shifting dullness. There was palpable hepatomegaly but no splenomegaly. The lower extremities had bilateral pitting edema, tenderness and erythema.
Routine laboratory tests showed a platelet count of 754 k/µL, white blood cell count 12.4 k/µL, serum sodium level 128 mEq/L, alanine aminotransferase 93 U/L, aspartate aminotransferase 871 U/L, total serum bilirubin 4.3 mg/dL, direct serum bilirubin 2.8 mg/dL and albumin 2.6 g/dL. His alpha fetoprotein (AFP) level was 79,102 ng/mL, and thrombopoietin level was 126 pg/mL. JAK2 mutation was negative and no other cause of reactive thrombocytosis could be identified. One year prior to this admission, the patient was noted to have a normal platelet count and AFP level. Results of laboratory parameters are given in Table 1.
 Click to view | Table 1. Initial Laboratory Workup |
Computed tomography of the abdomen and pelvis revealed hepatomegaly with numerous hypodensities suspicious for HCC (Fig. 1). Abdominal paracentesis was done, serum ascites albumin gradient (SAAG) was 2.4 g/dL consistent with portal hypertension, total protein was 1.2 g/dL, ascetic fluid white blood cell count was 440 cells/mL and the neutrophil count was 30 cells/mL. Spontaneous bacterial peritonitis (SBP) was ruled out. Magnetic resonance imaging of the liver was consistent with infiltrating HCC, portal vein thrombosis and retroperitoneal lymphadenopathy (Fig. 2.). He was not considered a candidate for liver transplantation due to ongoing substance abuse. He was started on ciprofloxacin for SBP prophylaxis, lactulose, completed antibiotic treatment for cellulitis and was referred to oncology. He expired 1 month later.
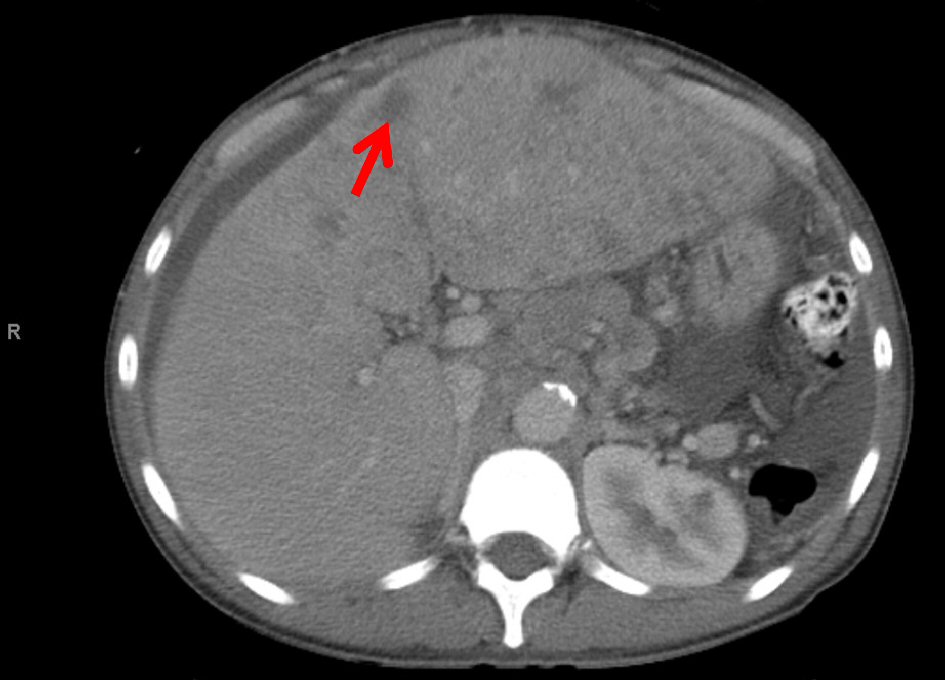 Click for large image | Figure 1. CT of the abdomen and pelvis reveals hepatomegaly with numerous hypodensities suspicious for HCC. |
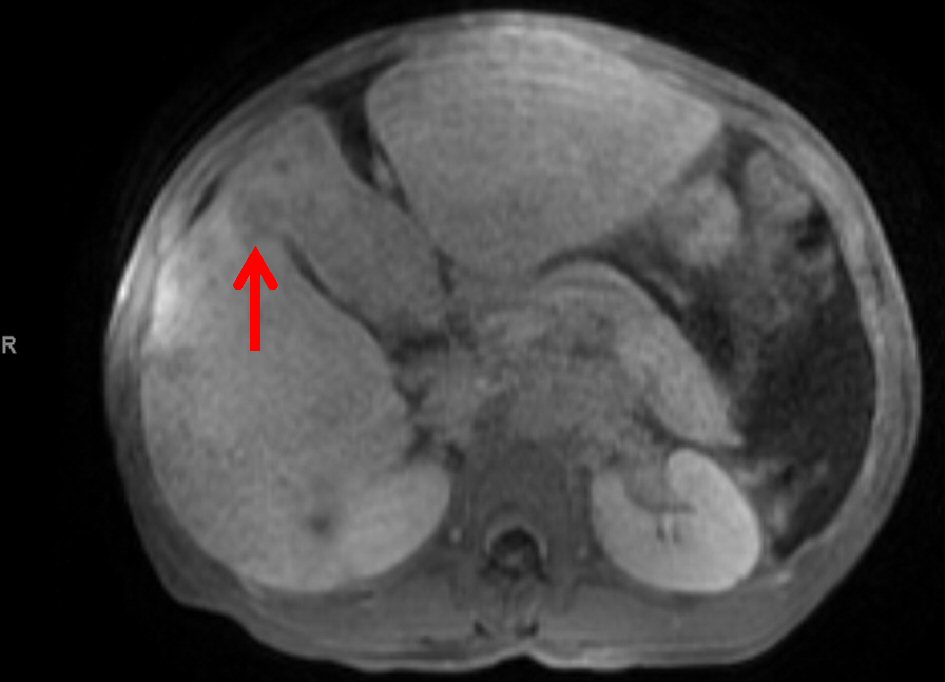 Click for large image | Figure 2. MRI of the abdomen and pelvis reveals abnormal T1 low appearance of the anterior segment of the right hepatic lobe and left hepatic lobe, and heterogeneous appearance of the right hepatic lobe with several hypointense foci on T1-weighted series. |
| Discussion | ▴Top |
HCC is a highly malignant tumor that occurs in the background of chronic inflammation and liver injury due to hepatitis B, C, chronic alcohol use, hemochromatosis or non-alcoholic fatty liver disease (NAFLD) [4]. It is mostly associated with cirrhosis, but in case of hepatitis B infection, HCC can develop without developing cirrhosis. Long standing infection with hepatitis B increases the risk of HCC considerably as compared to the uninfected individuals, while in the presence of macronodular cirrhosis the risk of HCC is increased by 10-fold [6, 7]. Hepatitis B belongs to the Hepadnaviridae family and has direct oncogenic effects [8], and can cause HCC in the absence of micro or macro nodular cirrhosis. On the contrary hepatitis C causes HCC in the setting of cirrhosis only in most cases, and effective treatment and eradication of hepatitis C virus before cirrhosis development results in decreased risk of subsequent HCC [9]. The risk of HCC in HCV-infected individuals is 20 times higher as compared to non-infected individuals [10]. There are many paraneoplastic syndromes that manifest in the presence of HCC and the prevalence of paraneoplastic syndrome in HCC is 27% according to one study [11], and as high as 43% according to another [12]. These include erythrocytosis, hypercholesterolemia, hypercalcemia, hypoglycemia, demyelinating disease, pemphigus, polyarthritis, encephalomyelitis, and thrombocytosis [5, 11, 13-20]. Hypercholesterolemia, hypercalcemia, and erythrocytosis occur more commonly than others [21], and according to one study their prevalence is 24.5%, 5.3%, and 3.9%, respectively [11]. Paraneoplastic syndromes in HCC are seen in advanced disease, advanced TNM staging at diagnosis and higher AFP levels [11].
Thrombocytosis is a rare paraneoplastic condition seen in HCC [4, 5, 22, 23]. Human thrombopoietin (TPO) or the megakaryocyte growth factor is secreted by both hepatocytes and bone marrow cells [24, 25]. It is hypothesized that the thrombocytosis seen in association with HCC is secondary to increased production of TPO by the tumor cells [5]. Thrombocytosis in HCC is associated with a high tumor burden, portal vein thrombosis (PVT), serum AFP levels and a poor prognosis [5].
Our case is unique as we observed all features including an elevated level of TPO, high AFP levels, and PVT associated with thrombocytosis and a poor prognosis in HCC. Thrombocytosis in a cirrhotic patient should alert the presence of HCC, and when present is an indicator of poor outcomes.
Disclosure
None.
Abbreviations
HCC: hepatocellular carcinoma; TPO: thrombopoietin; CTP: Child-Turcotte-Pugh; MELD: model for end-stage liver disease; AFP: alpha fetoprotein; SBP: spontaneous bacterial peritonitis; NAFLD: non-alcoholic fatty liver disease; PVT: portal vein thrombosis
| References | ▴Top |
- Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94(2):153-156.
doi pubmed - Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat database: incidence - SEER 9 Regs research data, Nov 2009 Sub (1973-2007). Bethesda, MD: National Cancer Institute, April 2010.
- El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365(12):1118-1127.
doi pubmed - Carr BI, Guerra V. Thrombocytosis and hepatocellular carcinoma. Dig Dis Sci. 2013;58(6):1790-1796.
doi pubmed - Hwang SJ, Luo JC, Li CP, Chu CW, Wu JC, Lai CR, Chiang JH, et al. Thrombocytosis: a paraneoplastic syndrome in patients with hepatocellular carcinoma. World J Gastroenterol. 2004;10(17):2472-2477.
doi pubmed - Robinson WS. The role of hepatitis B virus in the development of primary hepatocellular carcinoma: Part I. J Gastroenterol Hepatol. 1992;7(6):622-638.
doi pubmed - Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet. 1981;2(8256):1129-1133.
doi - Ringelhan M, O'Connor T, Protzer U, Heikenwalder M. The direct and indirect roles of HBV in liver cancer: prospective markers for HCC screening and potential therapeutic targets. J Pathol. 2015;235(2):355-367.
doi pubmed - Lim EJ, Torresi J. Prevention of hepatitis C virus infection and liver cancer. Recent Results Cancer Res. 2014;193:113-133.
doi pubmed - Sun CA, Wu DM, Lin CC, Lu SN, You SL, Wang LY, Wu MH, et al. Incidence and cofactors of hepatitis C virus-related hepatocellular carcinoma: a prospective study of 12,008 men in Taiwan. Am J Epidemiol. 2003;157(8):674-682.
doi pubmed - Chang PE, Ong WC, Lui HF, Tan CK. Epidemiology and prognosis of paraneoplastic syndromes in hepatocellular carcinoma. ISRN Oncol. 2013;2013:684026.
doi - Huh UY, Kim JH, Kim BH, Nam KD, Jang JY, Kim NH, Lee SK, et al. [The incidence and clinical significance of paraneoplastic syndromes in patients with hepatocellular carcinoma]. Korean J Hepatol. 2005;11(3):275-283.
pubmed - Goldberg RB, Bersohn I, Kew MC. Hypercholesterolaemia in primary cancer of the liver. S Afr Med J. 1975;49(36):1464-1466.
pubmed - Sorlini M, Benini F, Cravarezza P, Romanelli G. Hypoglycemia, an atypical early sign of hepatocellular carcinoma. J Gastrointest Cancer. 2010;41(3):209-211.
doi pubmed - Oldenburg WA, van Heerden JA, Sizemore GW, Abboud CF, Sheedy PF, 2nd. Hypercalcemia and primary hepatic tumors. Arch Surg. 1982;117(10):1363-1366.
doi pubmed - Chang PE, Tan CK. Paraneoplastic erythrocytosis as a primary presentation of hepatocellular carcinoma. Indian J Med Sci. 2009;63(5):202-203.
doi pubmed - Walcher J, Witter T, Rupprecht HD. Hepatocellular carcinoma presenting with paraneoplastic demyelinating polyneuropathy and PR3-antineutrophil cytoplasmic antibody. J Clin Gastroenterol. 2002;35(4):364-365.
doi pubmed - Arguedas MR, McGuire BM. Hepatocellular carcinoma presenting with chronic inflammatory demyelinating polyradiculoneuropathy. Dig Dis Sci. 2000;45(12):2369-2373.
doi - Hinterhuber G, Drach J, Riedl E, Bohler K, Ferenci P, Wolff K, Foedinger D. Paraneoplastic pemphigus in association with hepatocellular carcinoma. J Am Acad Dermatol. 2003;49(3):538-540.
doi - Coeytaux A, Kressig R, Zulian GB. Hepatocarcinoma with concomitant paraneoplastic encephalomyelitis. J Palliat Care. 2001;17(1):59-60.
pubmed - Luo JC, Hwang SJ, Wu JC, Li CP, Hsiao LT, Lai CR, Chiang JH, et al. Paraneoplastic syndromes in patients with hepatocellular carcinoma in Taiwan. Cancer. 1999;86(5):799-804.
doi - Ryu T, Nishimura S, Miura H, Yamada H, Morita H, Miyazaki H, Kitamura S, et al. Thrombopoietin-producing hepatocellular carcinoma. Intern Med. 2003;42(8):730-734.
doi pubmed - Chen CC, Chang JY, Liu KJ, Chan C, Ho CH, Lee SC, Chen LT. Hepatocellular carcinoma associated with acquired von Willebrand disease and extreme thrombocytosis. Ann Oncol. 2005;16(6):988-989.
doi pubmed - de Sauvage FJ, Hass PE, Spencer SD, Malloy BE, Gurney AL, Spencer SA, Darbonne WC, et al. Stimulation of megakaryocytopoiesis and thrombopoiesis by the c-Mpl ligand. Nature. 1994;369(6481):533-538.
doi pubmed - Lok S, Kaushansky K, Holly RD, Kuijper JL, Lofton-Day CE, Oort PJ, Grant FJ, et al. Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature. 1994;369(6481):565-568.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


