Figures
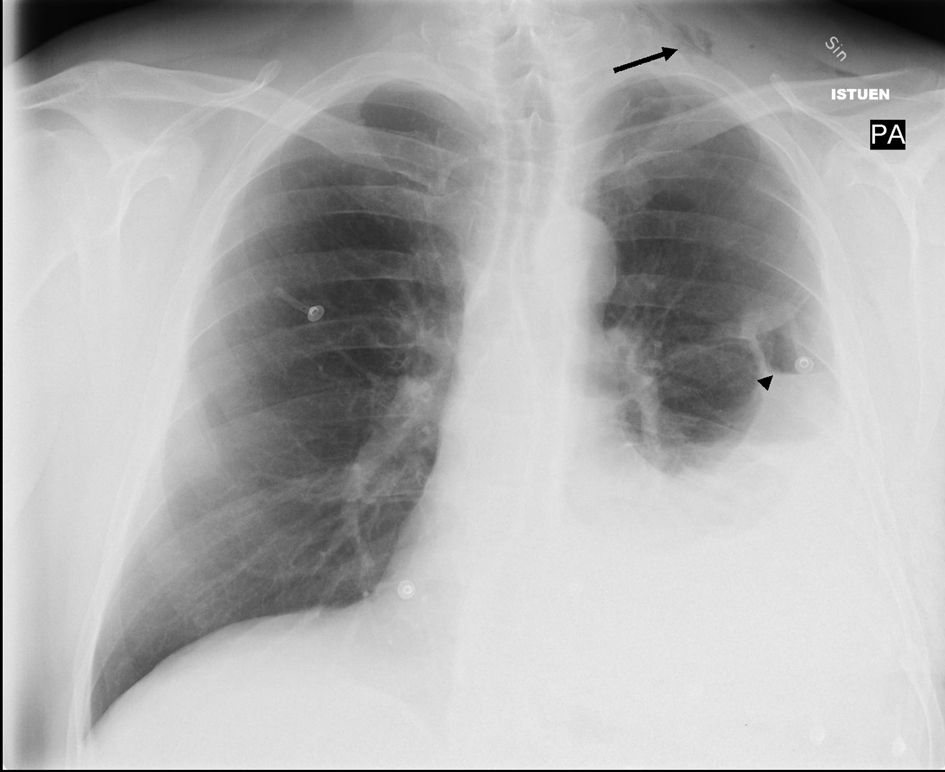
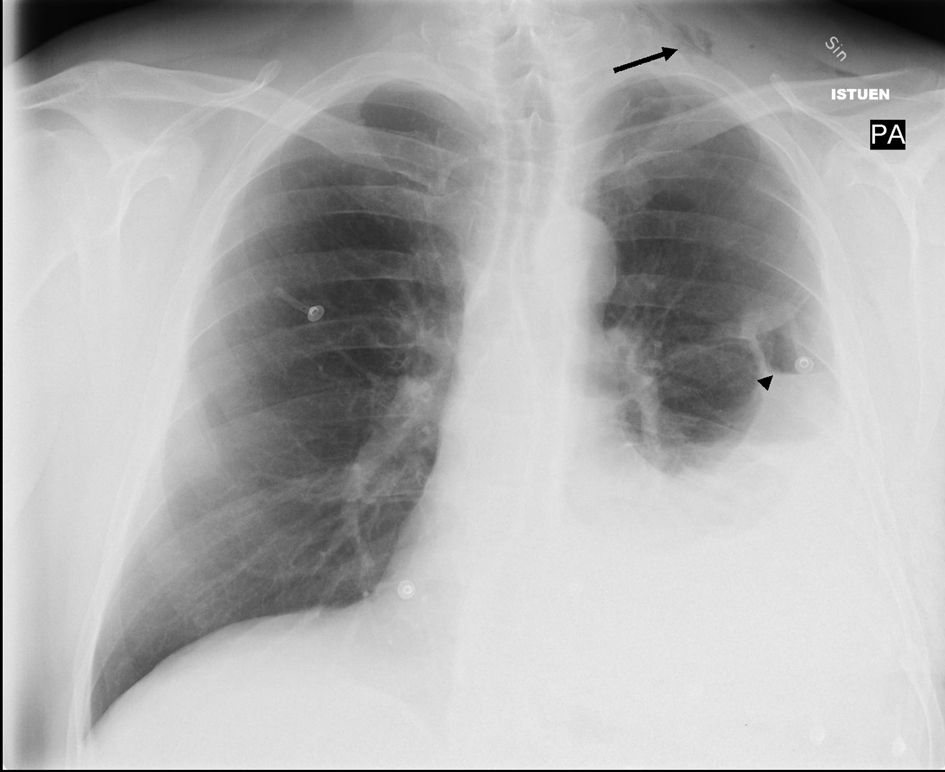
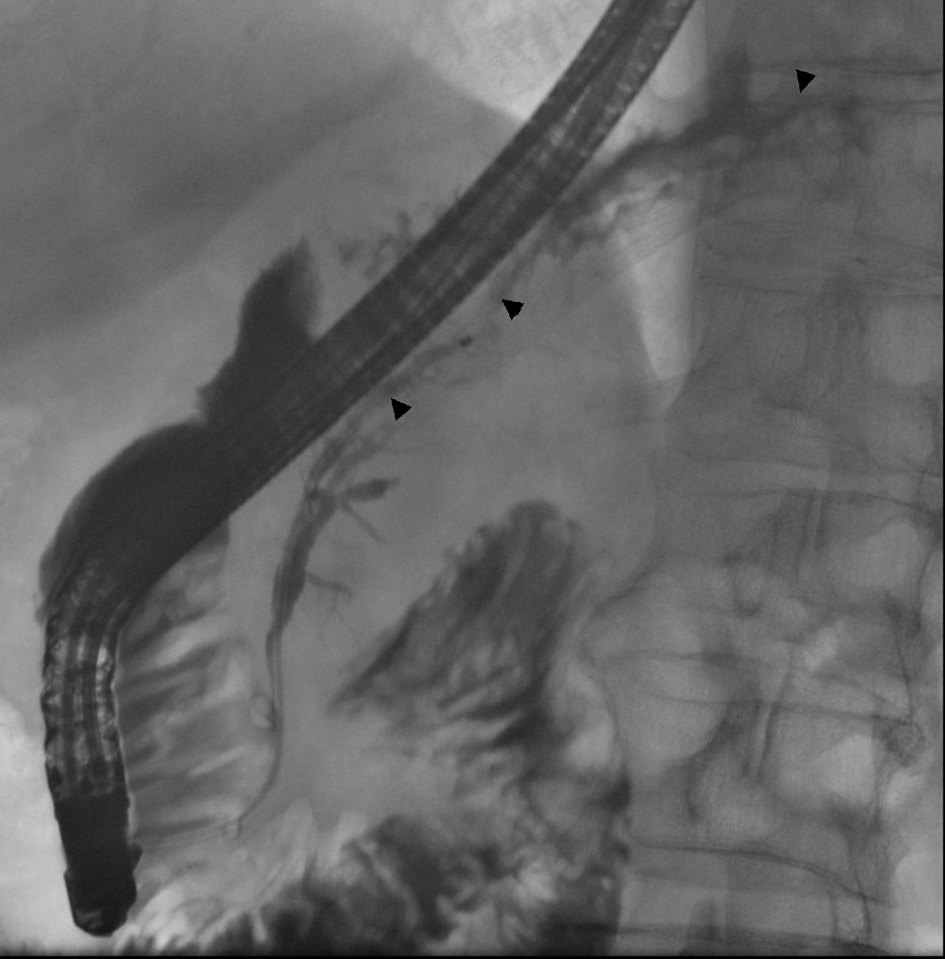
Figure 1. Chest X-ray showing left-sided pleural effusion with a small apical pneumothorax indicative of a hemo-pneumothorax. Note subcutaneous air in left jugular region (arrow) and a small air-fluid level (arrowhead).
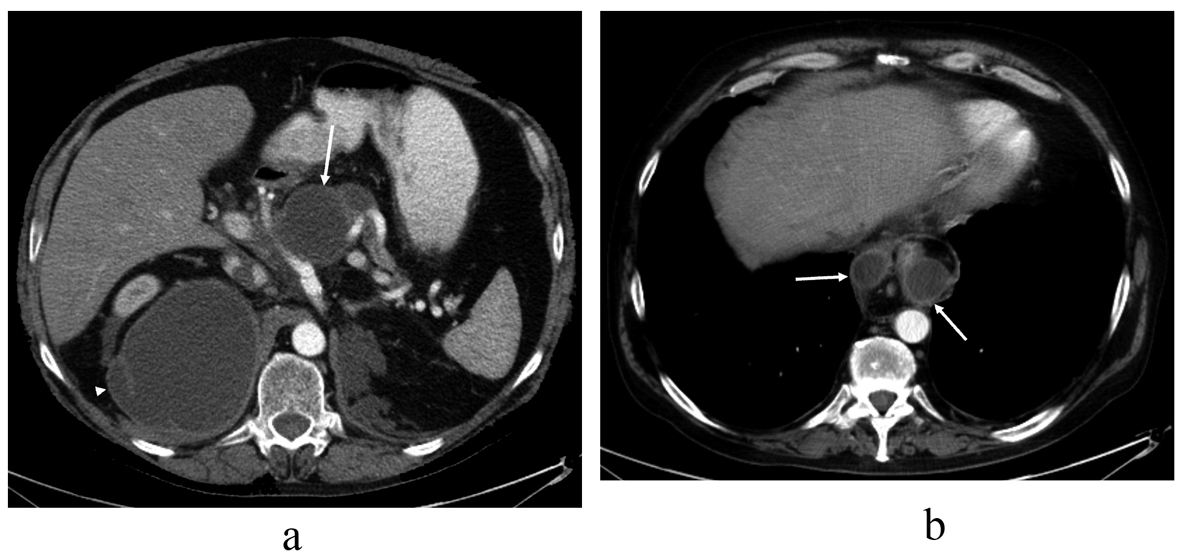
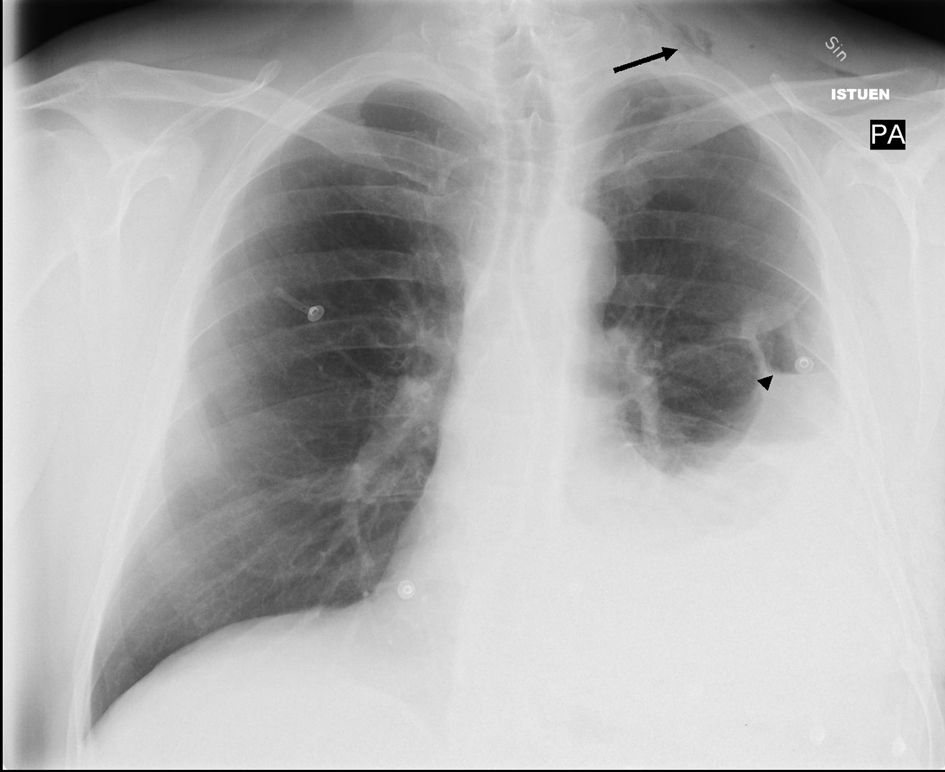
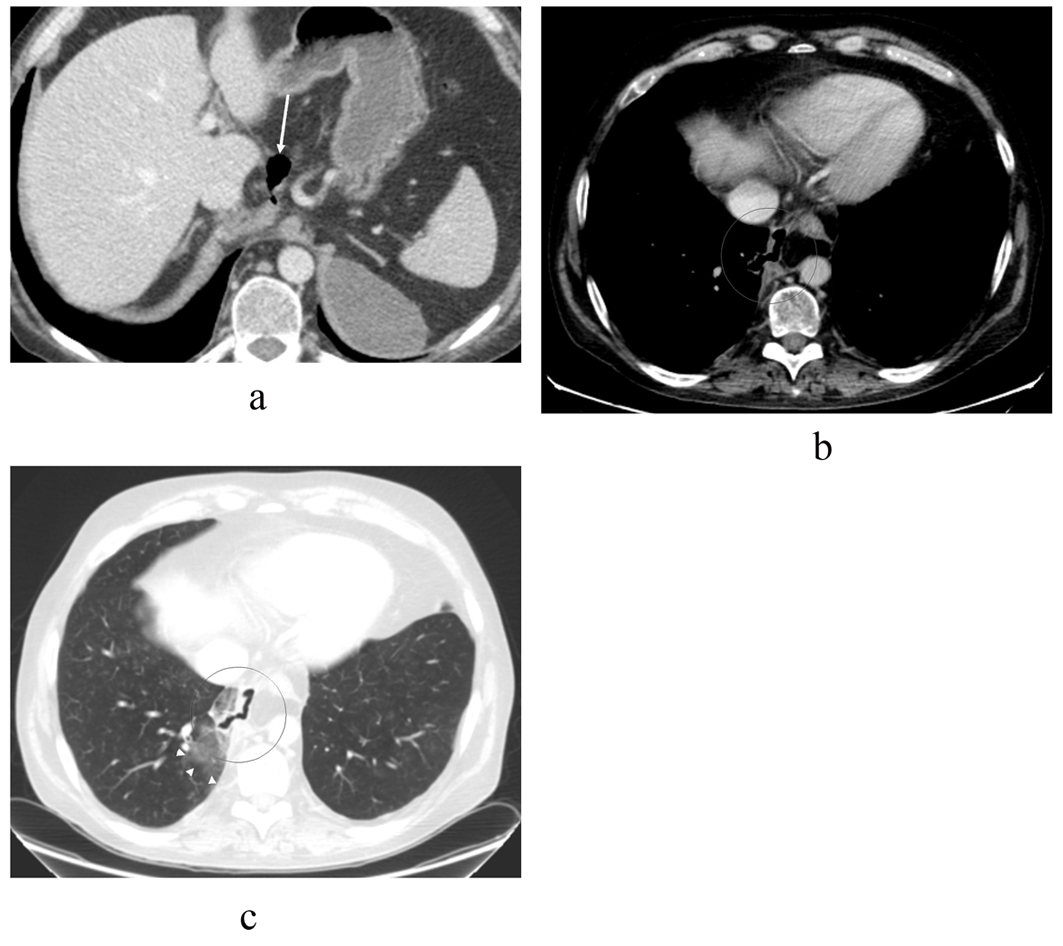
Figure 2. Contrast-enhanced abdominal CT image taken over 1.5 years after the thoracic injury, revealing (a) communicating fluid collections above the pancreas (arrow) and in the right subphrenic space (arrowhead) with wall enhancement. There is also a small separate fluid collection in the left subphrenic space indicative for old hematoma. The pancreas shows atrophy but there are no parenchymal calcifications or peripancreatic edema, so there is no evidence of acute or chronic pancreatitis. In the upper level (b) the pseudocysts (arrows) rise up through the hiatus opening to the mediastinum surrounding the esophagus. At this time, the lung parenchyma was normal. No pleural effusion is seen.
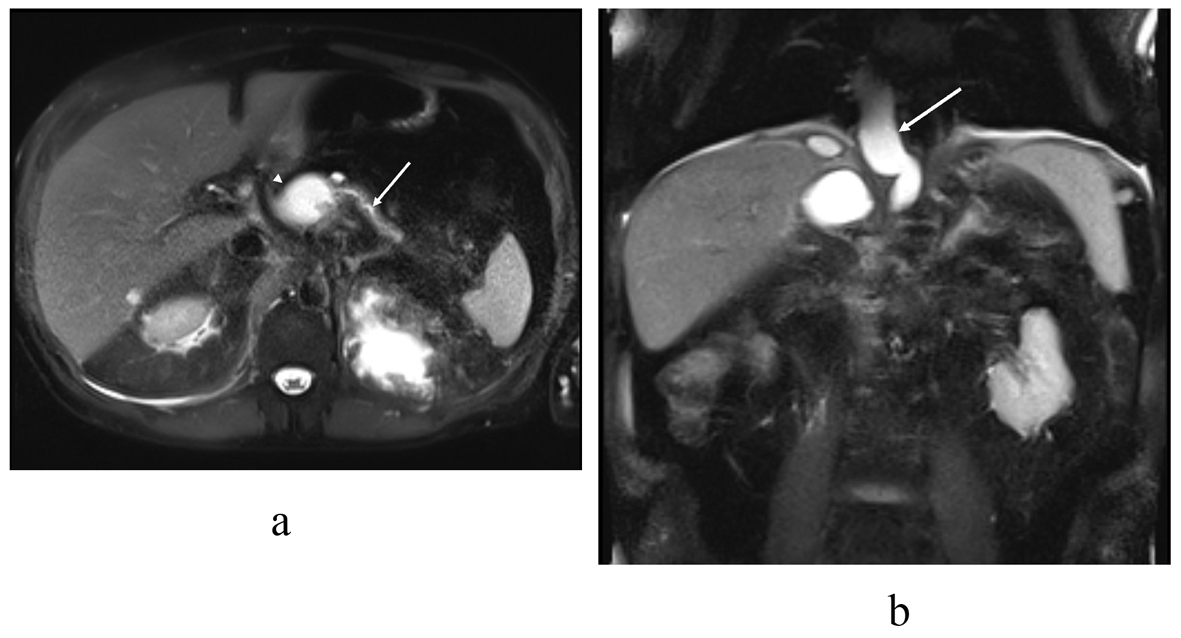
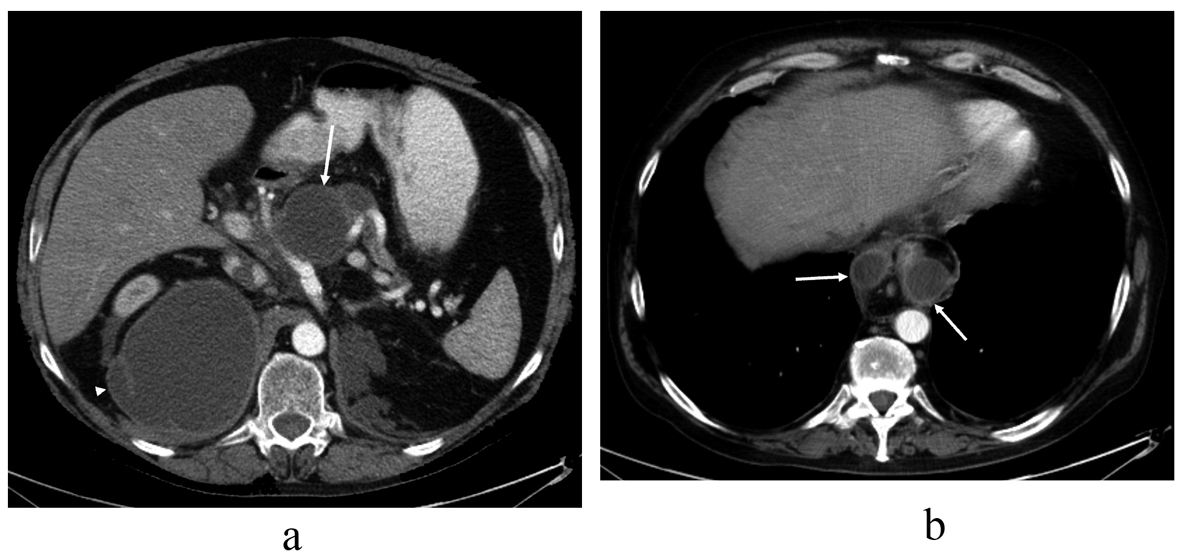
Figure 3. T2 (haste) MRI in the (a) transaxial and (b) coronal plane demonstrates the distal pancreatic duct (arrow) communicating with the pancreatic body pseudocyst (arrowhead). In the coronal plane (b) a pseudocyst (arrow) extends through the hiatus opening to the mediastinum, similar to the previous CT scan.
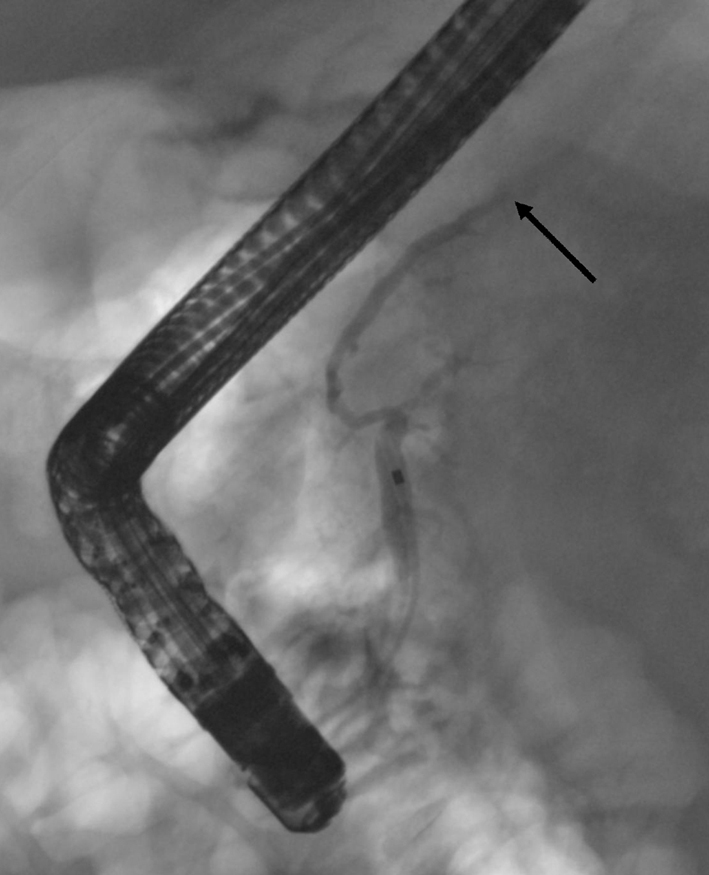
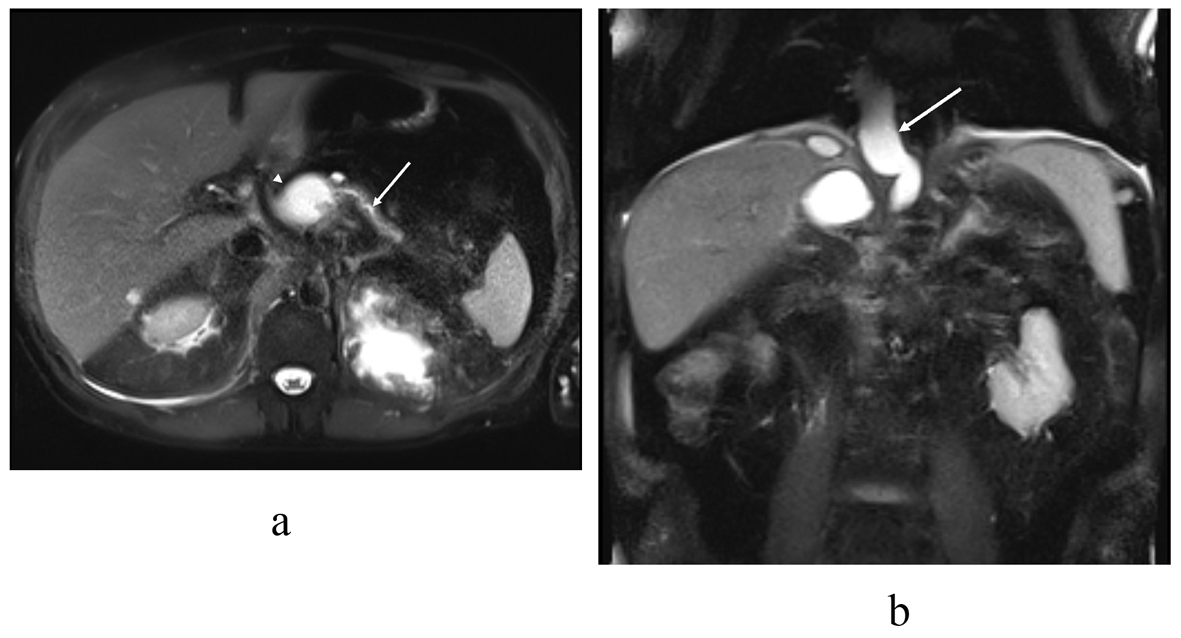
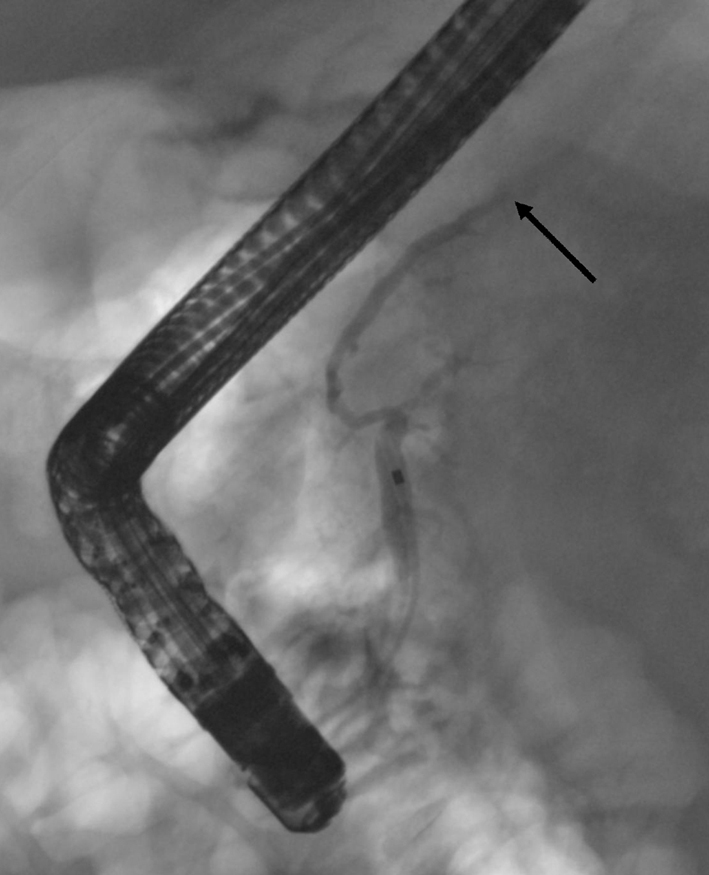
Figure 4. In the first ERCP the cannula is in the pancreatic duct. The duct appears normal at the head and the body but within the body-tail junction the duct is interrupted (arrow) and no contrast is seen in the pancreatic tail duct. No contrast leakage is seen at this time.
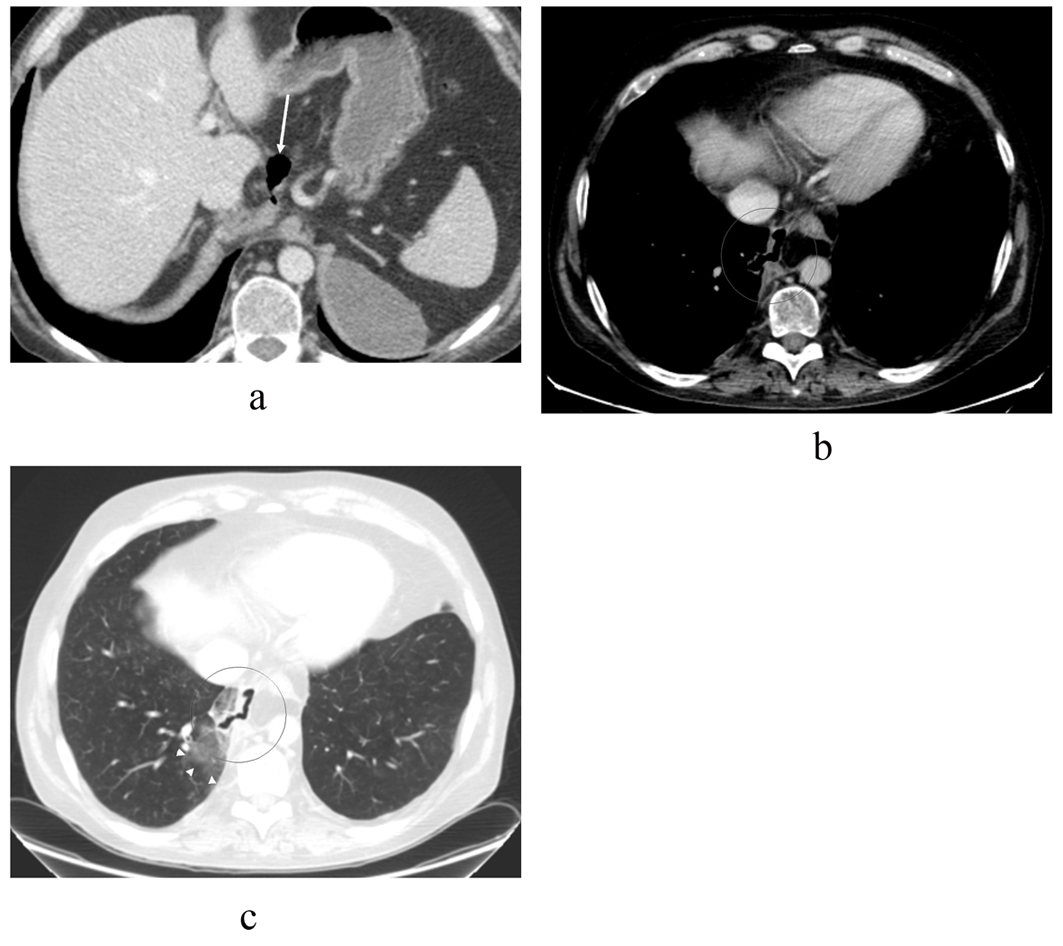
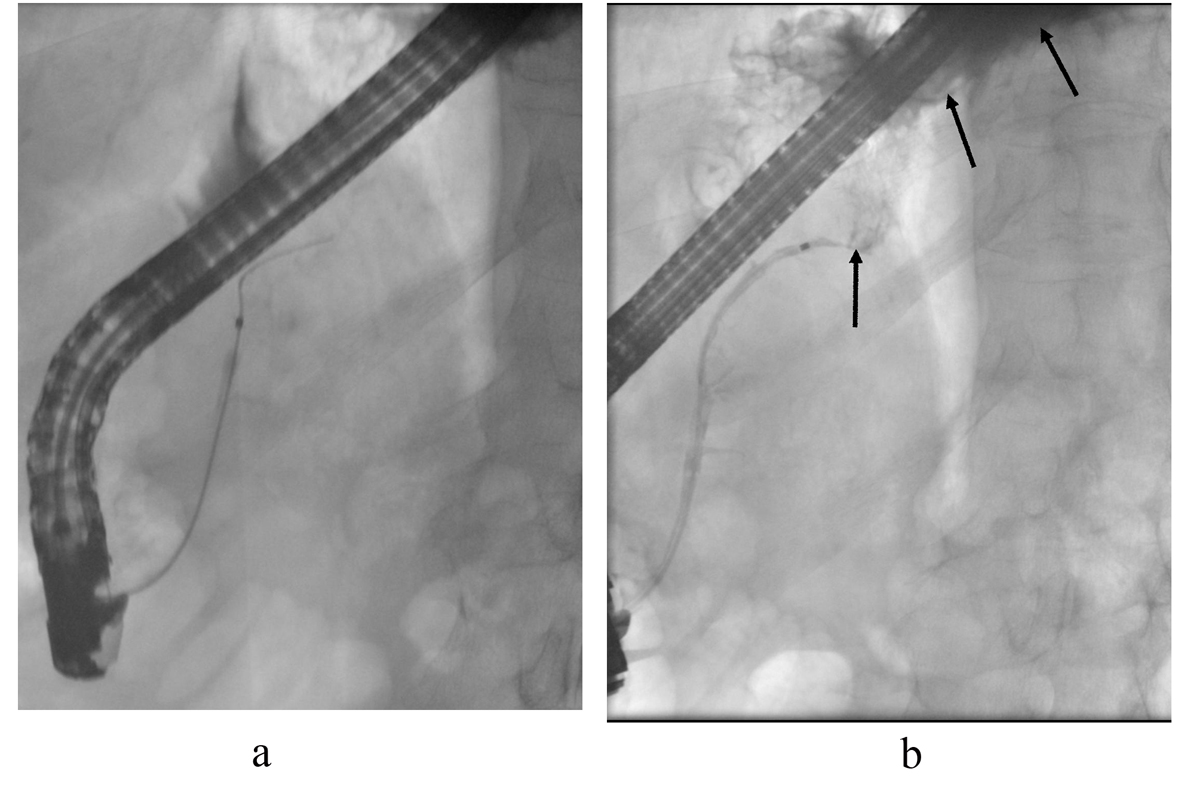
Figure 5. CT scan images taken 4 months after the primary ERCP shows that the pseudocysts have retreated (a) compared to previous CT and MRCP scans (Fig. 2, 3) but there is an air-filled passage above the pancreas (arrow), which protrudes in to the mediastinum. The separate left subphrenic hematoma is still visible. In the upper level with (b) mediastinal and (c) lung window settings the air-filled channel penetrates through the right mediastinal pleura in to the lung parenchyma where there is some ground-glass opacity (arrowheads) indicative of parenchymal irritation. No pleural effusion is seen.
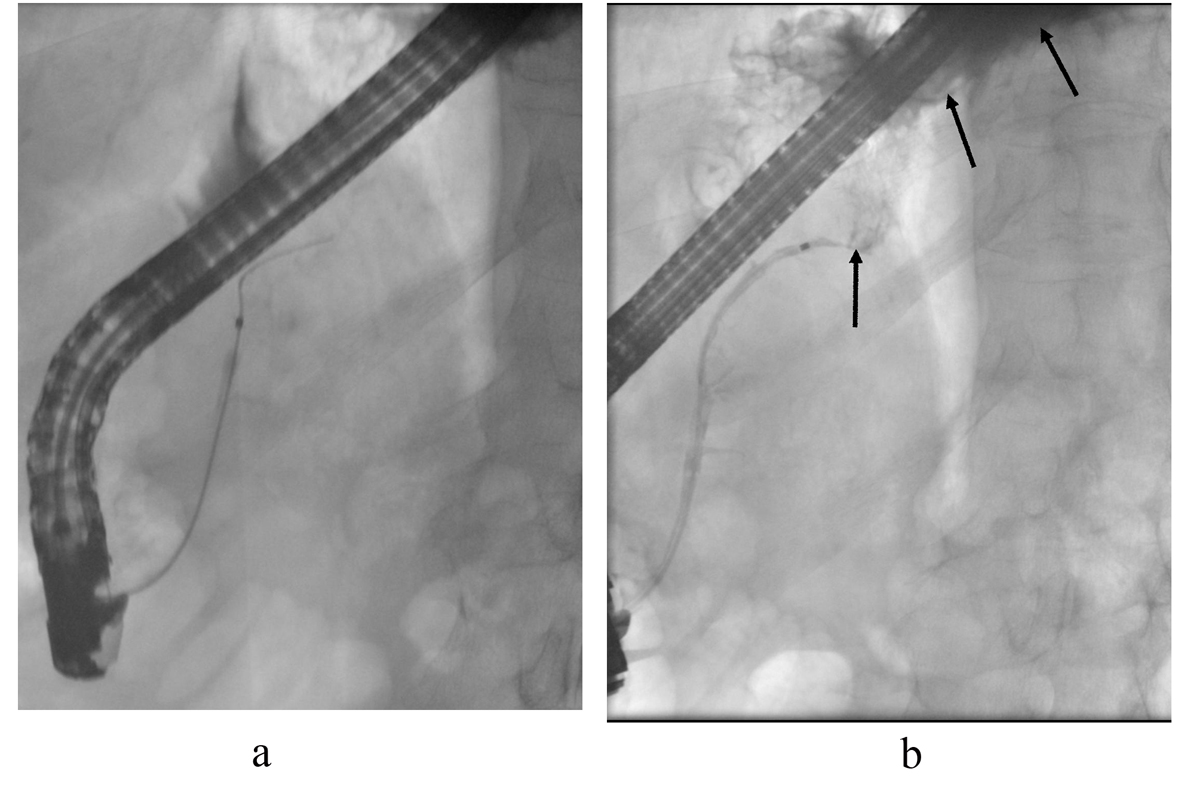
Figure 6. ERCP control images. The cannula is in the pancreatic duct. (a) After contrast injection, contrast leakage is seen above the pancreatic body (arrows) filling the mediastinal pseudocyst (b). The pancreatic duct was stented.
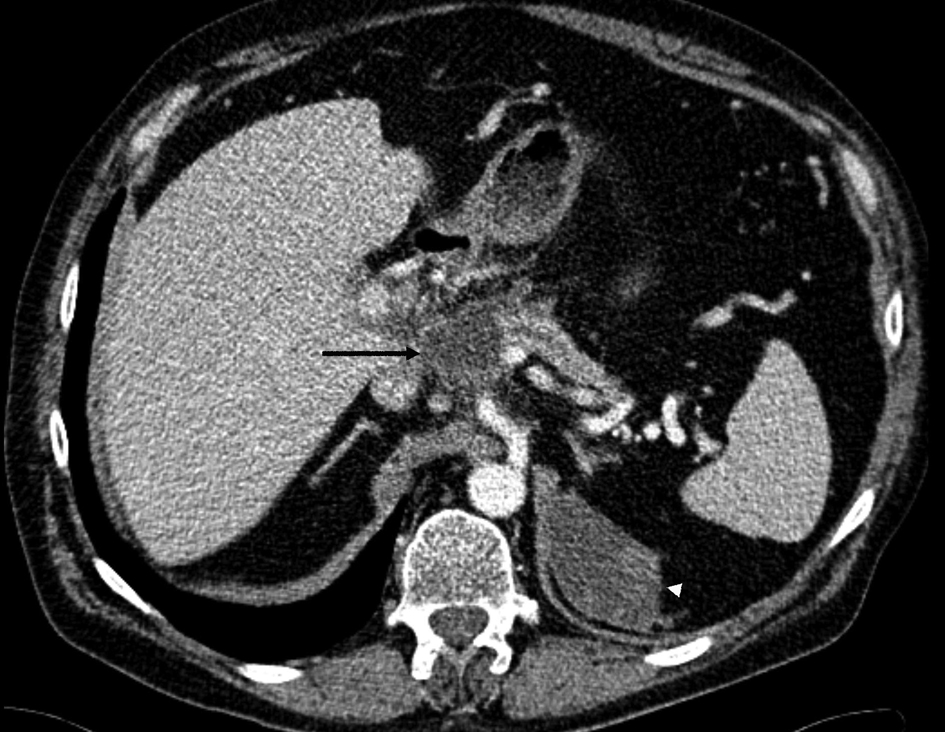
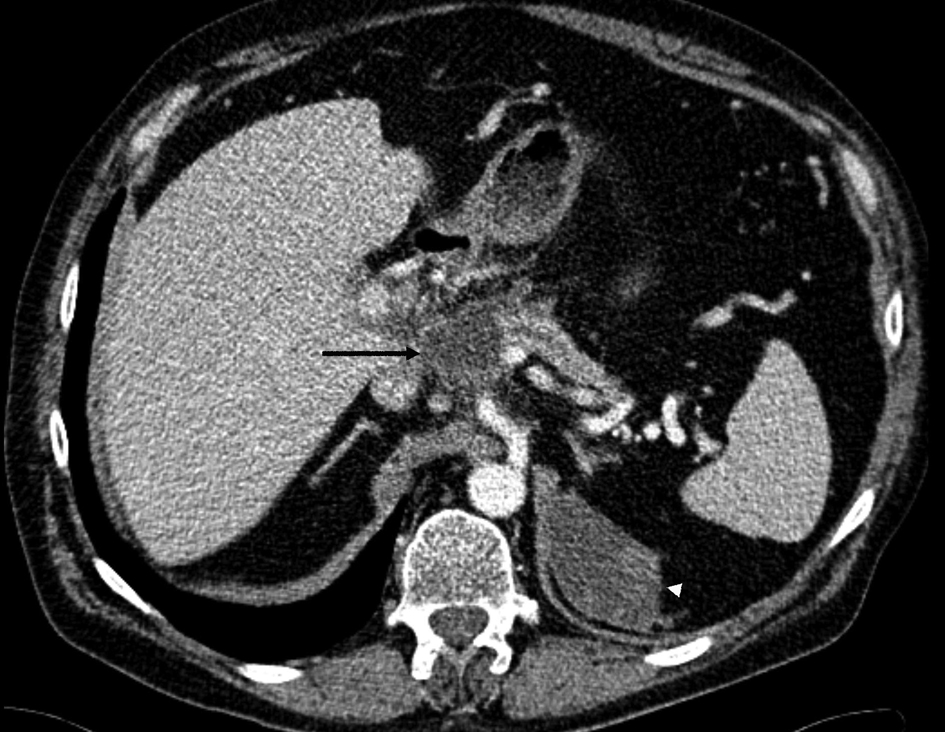
Figure 7. A contrast-enhanced CT scan image shows a small 4.3 cm residual pseudocyst (arrow) above the pancreatic body adjacent to the normal caliber pancreatic duct. There is peripancreatic edema indicative for acute pancreatitis. The left subphrenic chronic hematoma is slowly shrinking (arrowhead).
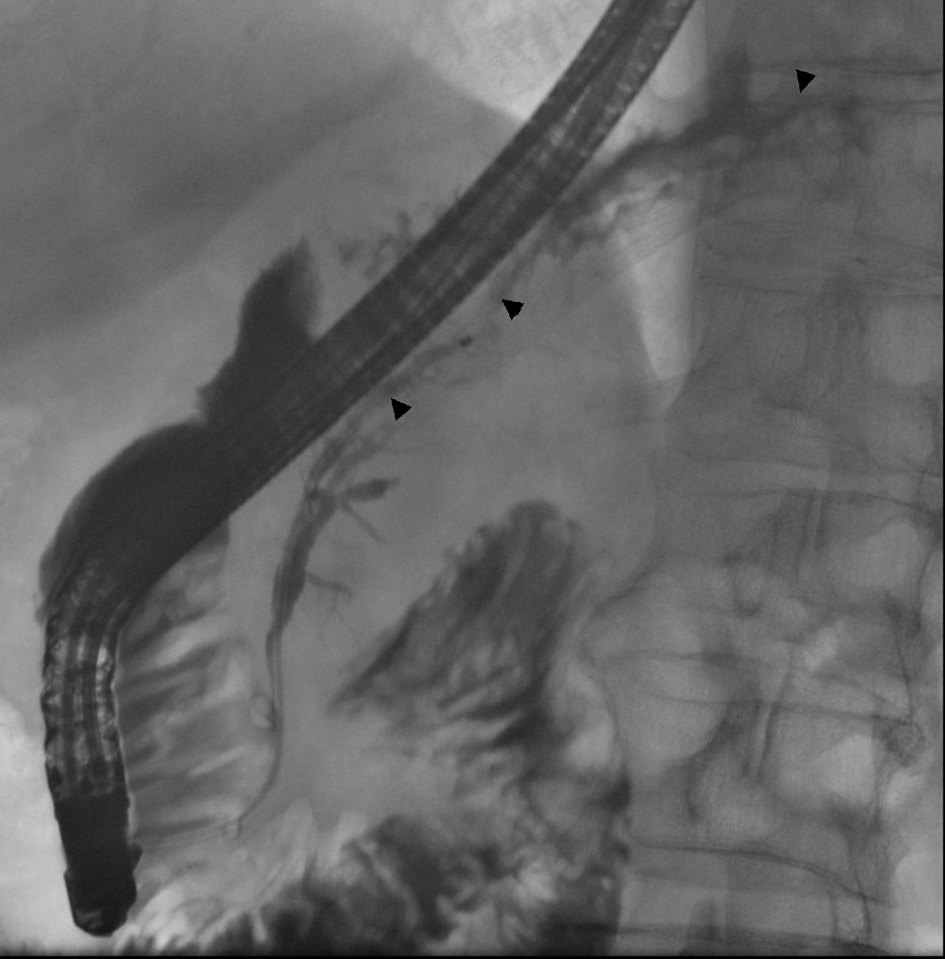
Figure 8. In ERCP control images, a normal pancreatic duct is seen (arrowheads) as there is no interruption in the body-tail junction and the duct of the tail fills normally. There is no sign of obvious contrast leakage. The stent has been removed.

Figure 9. Latest CT scan image taken in the Central Hospital without contrast media shows that the pseudocyst above the pancreatic body is stable (arrow) and no new fluid collections have emerged.