| Japan (Fujishiro M, 2009) [8] | • Aspirin, ticlopidine, and ethyl icosapentate were stopped 7 days before the procedures by most of the endoscopists, whereas warfarin was stopped 4 days before the procedures.
• With regard to the drug discontinuation before the procedures, no major differences were observed between a biopsy (low-risk procedure) and endoscopic mucosal resection (high-risk procedure).
• In case of higher risk of thromboembolism during the cessation of drugs, most of the endoscopists never performed a biopsy or endoscopic mucosal resection. |
| Korea (Lee SY, 2008) [1] | • Eastern endoscopists do not typically perform an endoscopic biopsy while their patients are on warfarin therapy.
• Eastern endoscopists restarted medications later (1 to 3 days) than Western endoscopists after a biopsy (same day).
• Eastern endoscopists do not perform a polypectomy while their patients are taking aspirin. They withdrew aspirin for more than 7 days before a polypectomy, and restarted it 1 to 3 days after a polypectomy. |
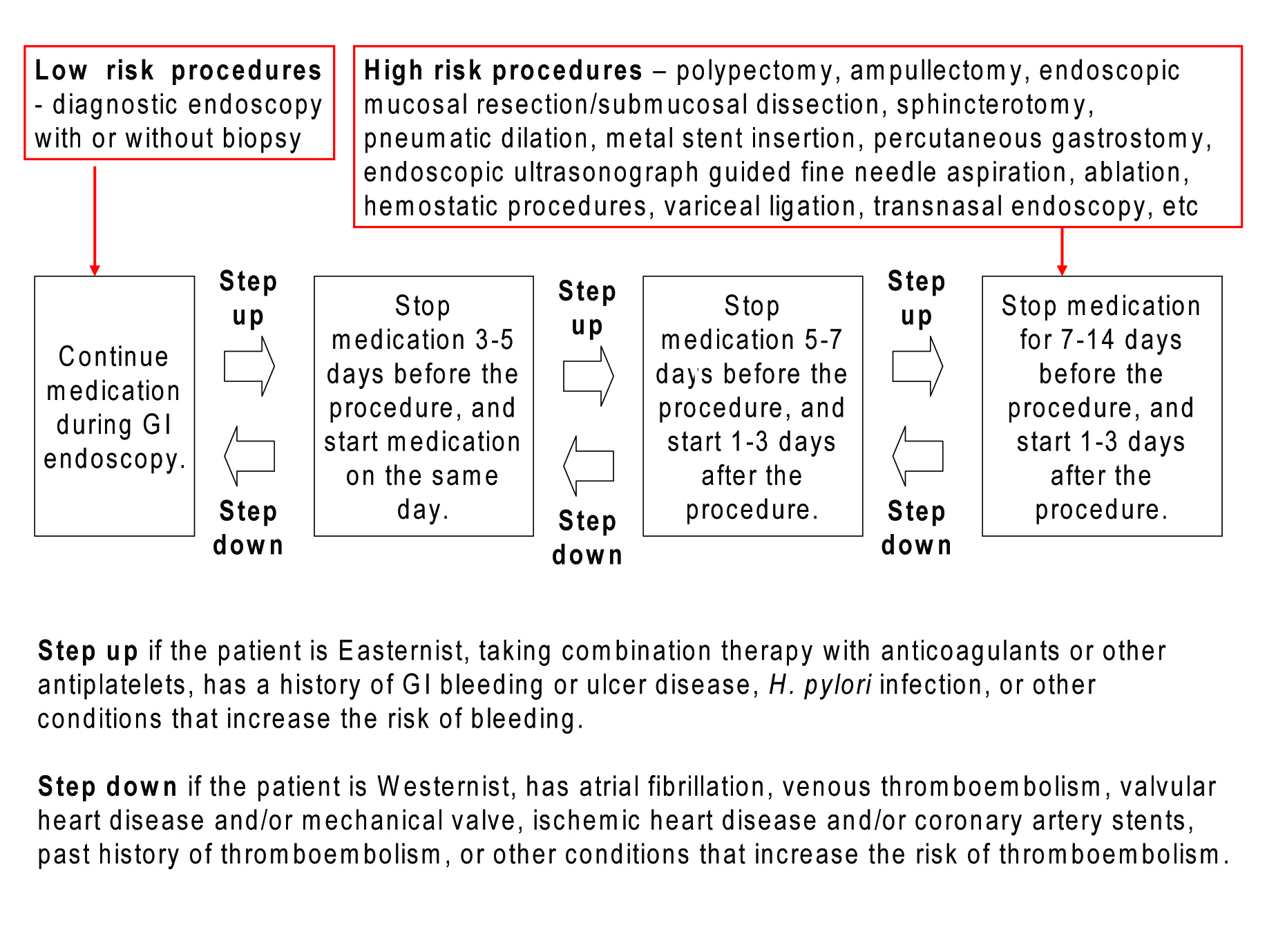
| UK (Veitch A, 2008) [5] | • Low-risk procedures can be performed during warfarin or clopidogrel intake.
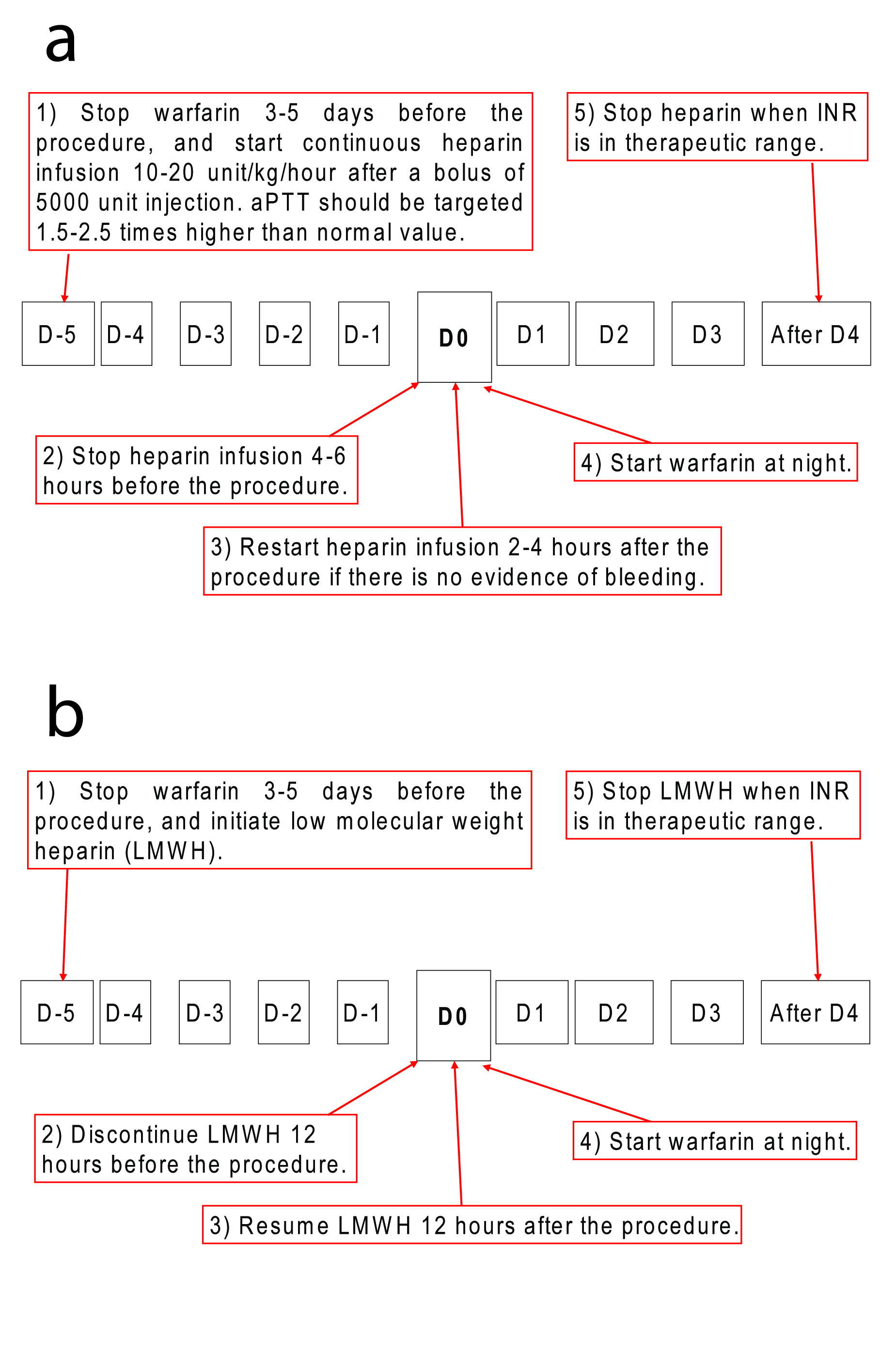
• High-risk procedures should be done after stopping warfarin for 5 days (INR < 1.5), and substituted with LMWH in high-risk conditions.
• In low-risk conditions, high-risk procedures can be performed after stopping clopidogrel for 7 days. Aspirin should be considered during the cessation of clopidogrel in such conditions.
• In high-risk conditions, continuing aspirin and stopping clopidogrel for 7 days should be considered, if 12 months have passed drug-eluting coronary stent insertion. |
| UK (Goel A, 2007) [10] | • With regard to warfarin, 26% of the endoscopists stopped for EGD, whereas 48.7% stopped for
colonoscopy.
• During warfarin intake, 21% took biopsies as usual, while 54% performed after checking the INR.
• Warfarin was usually stopped for 3 days. Preferred INR was below 2.0 during the endoscopic procedure. |
| Israel (Kimchi NA, 2007) [11] | • Aspirin can be continued for diagnostic EGD, but should be stopped 5 to 7 days before colonoscopy, spincterotomy, esophageal dilation, endoscopic ultrasound-guided biopsy, or drainage.
• Aspirin use should be avoided for 2 weeks after polypectomy, and 10 days after spincterotomy. However, when the cardiovascular risk is high, aspirin should be resumed within a week after the procedure.
• NSAIDs should be stopped 8 hours before any endoscopy, and be resumed 7 to 14 days after a high-risk procedure.
• Clopidogrel should be stopped 5 days before colonoscopy. |
| US (Makar GA, 2006) [12] | • For low-risk procedure (e.g. diagnostic endoscopy and colonoscopy without polypectomy), there is no need to discontinue or adjust anticoagulation.
• For high-risk procedures (e.g. polypectomy and biliary sphincterotomy), an individual approach is required. This approach includes stopping oral anticoagulant therapy with or without the administration of unfractionated heparin or LMWH during which the patient’s INR is in the subtherapeutic range.
• Antiplatelet therapy can be withheld for high risk procedures, but there is insufficient evidence to indicate that bleeding risk is impacted. |
| France (Naploen B, 2006) [4] | • Low-risk procedures can be performed during medications.
• High-risk procedures and transnasal endoscopy should be performed after the cessation of drugs.
• Colon polypectomy and endoscopic sphincterotomy could be performed without cessation of aspirin or NSAIDs. |
| Japan (Ogoshi K, 2005) [6] | • Warfarin should be stopped 3 to 4 days before all kinds of endoscopic procedure. INR less than 1.5 is preferred during the procedure.
• Aspirin should be stopped 3 days before low-risk procedures, and stopped 7 days before high-risk
procedures.
• Ticlopidine should be stopped 5 days before low-risk procedures, and stop 10 to 14 days before high-risk procedures.
• In case of dual antiplatelet intake (aspirin and ticlopidine), both antiplatelets should be stopped 7 days before low-risk procedures. |
| Germany (Mosler P, 2004) [13] | • Antiplatelets were usually continued before elective procedures including diagnostic EGD, colonoscopy, and ERCP.
• Aspirin and clopidogrel were more frequently stopped than NSAIDs prior to any endoscopic procedure.
• More than 80% stopped aspirin and clopidogrel before elective therapeutic endoscopic procedures.
• Warfarin was usually discontinued 3-5 days prior to the procedure, and was substituted with LMWH. |
| Belgium (Hittelet A, 2003) [14] | • It is not necessary to discontinue aspirin or NSAIDs for endoscopic procedures, when used in standard doses.
• It is not necessary to adjust anticoagulation for low-risk procedures, such as EGD, colonoscopy, ERCP with biopsy or stent insertion (without sphincterotomy).
• For ticlopidine or clopidogrel, it is prudent to discontinue 7 to 10 days for high-risk procedures.
• Warfarin should be discontinued 3 to 5 days before high-risk procedures. |
| US (Eisen G, 2002) [2] | • Any endoscopic procedure may be performed in patients taking aspirin or NSAIDs in the absence of pre-existing bleeding disorders.
• Discontinuation of oral anticoagulation is needed for high-risk endoscopic procedures.
• Consider a heparin window only for patients with high thromboembolic risk.
• Resumption of warfarin is generally recommended at the night of the procedure except for sphincterotomy. |
| US (Kadakia SC, 1996) [15] | • Physicians stopped aspirin and NSAIDs more frequently before colonoscopy and ERCP than before EGD.
• With aspirin or NSAIDs intake, cold biopsy or hot biopsy during EGD or colonoscopy was performed, but sphincterotomy was not.
• Optimal cessation period of aspirin or NSAIDs was less than 10 days.
• Warfarin was resumed immediately after diagnostic endoscopy, whereas 7 days of cessation period was observed after therapeutic endoscopy. |