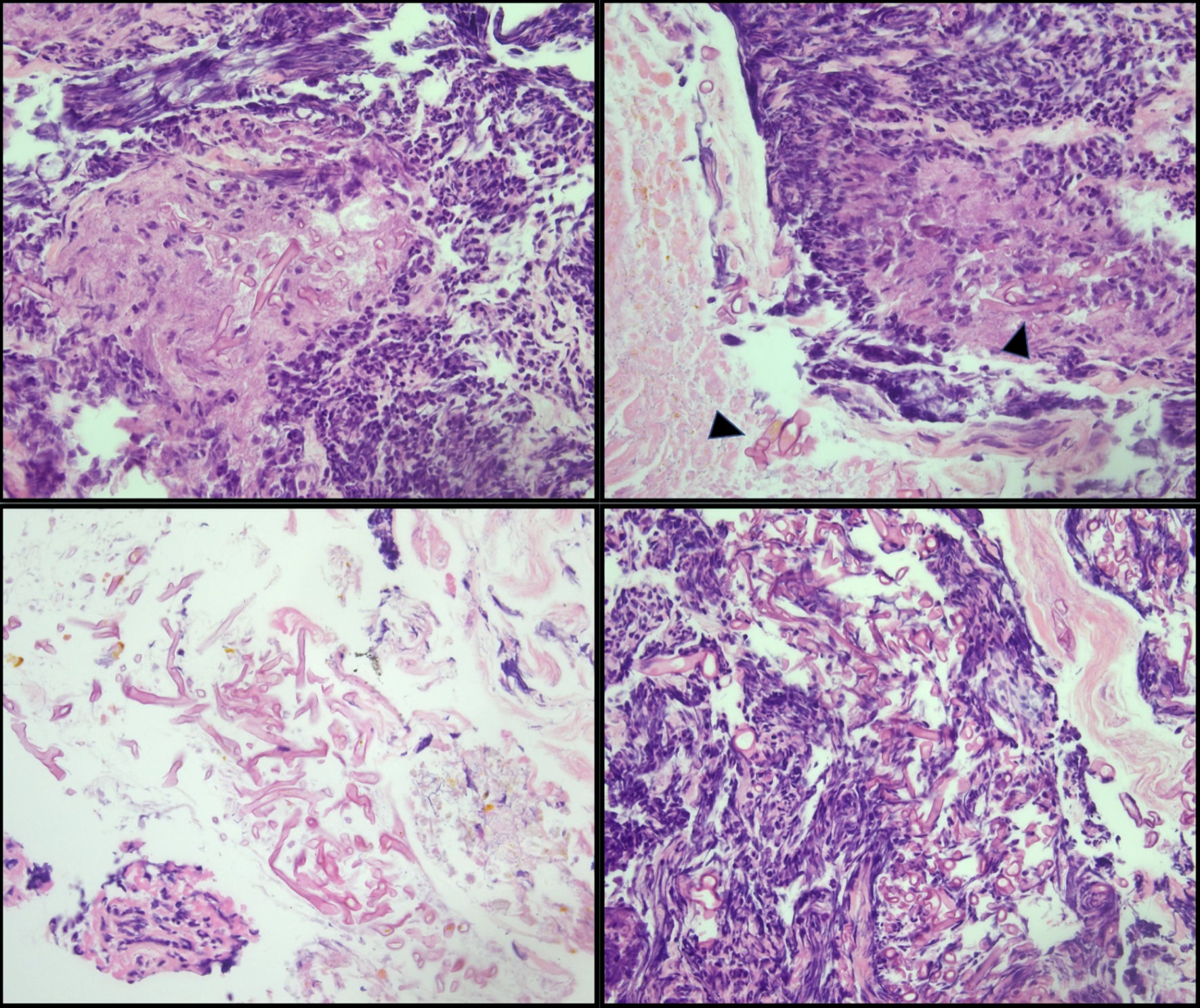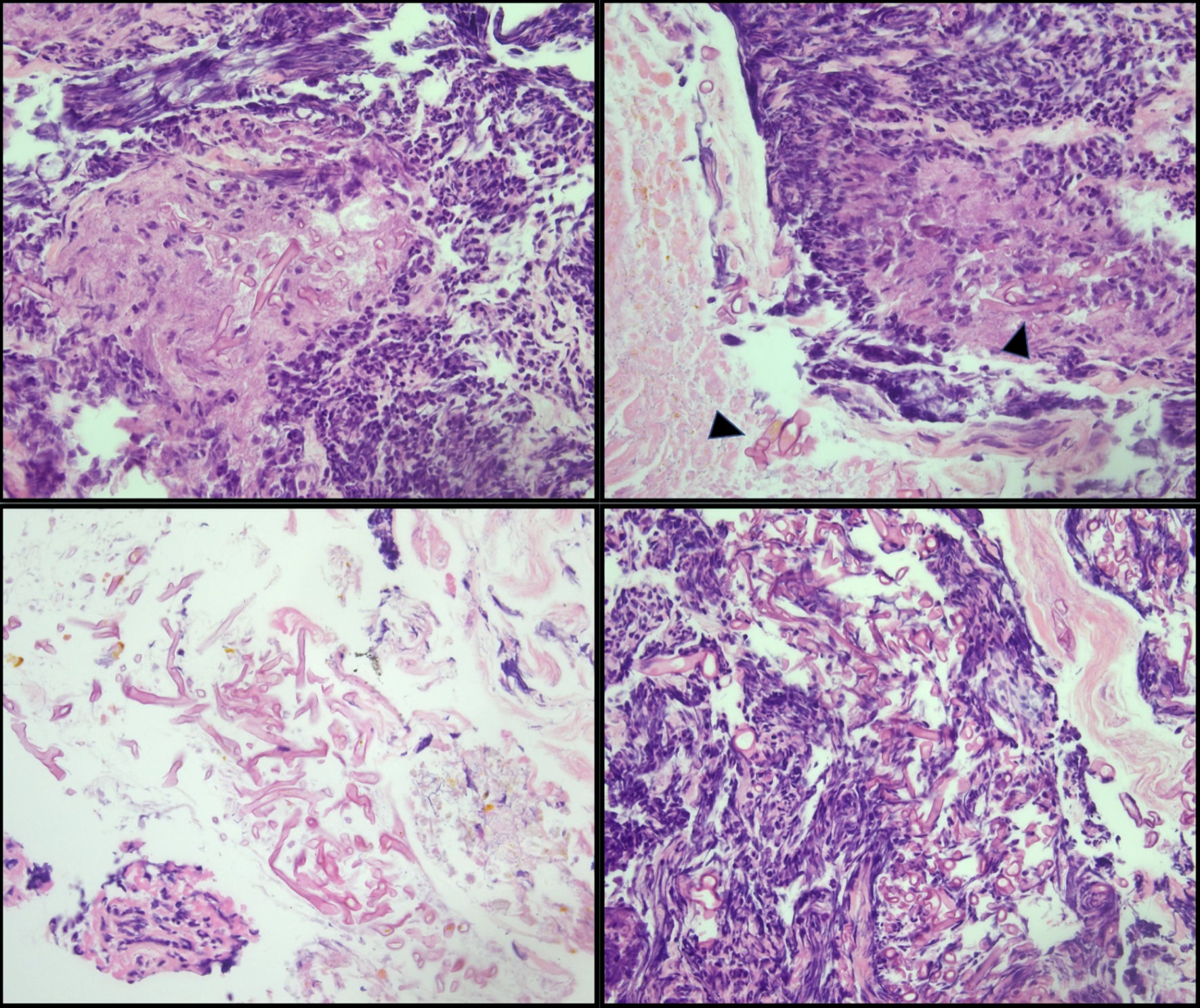
Figure 1. Cecal biopsy. Large, non-septate fungal organisms consistent with Mucorales (Mucor/Rhizopus) in a background of ulceration and acute inflammation (arrowhead). The presence of fungal organisms in the ulcer bed is most likely indicative of infection.
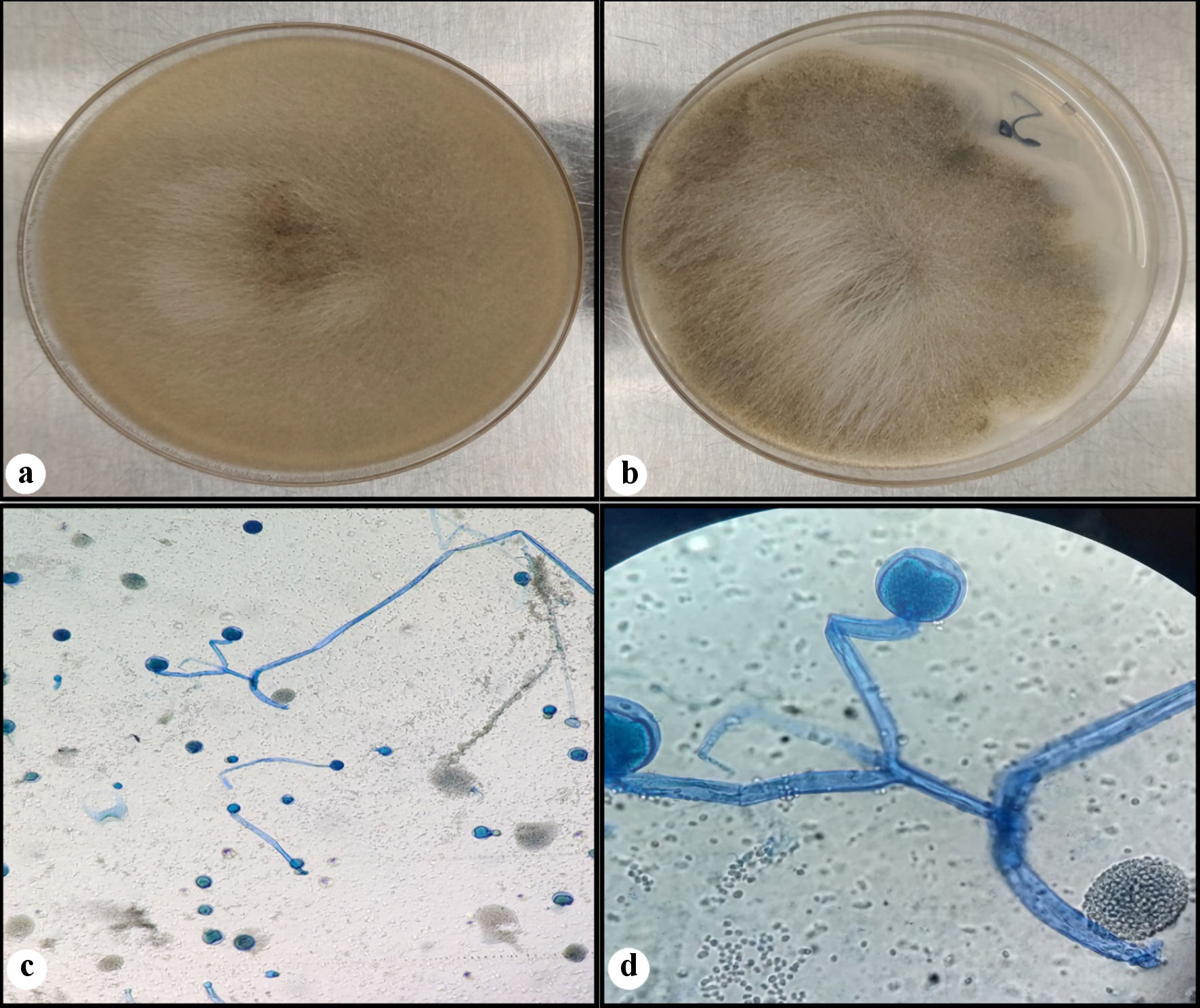
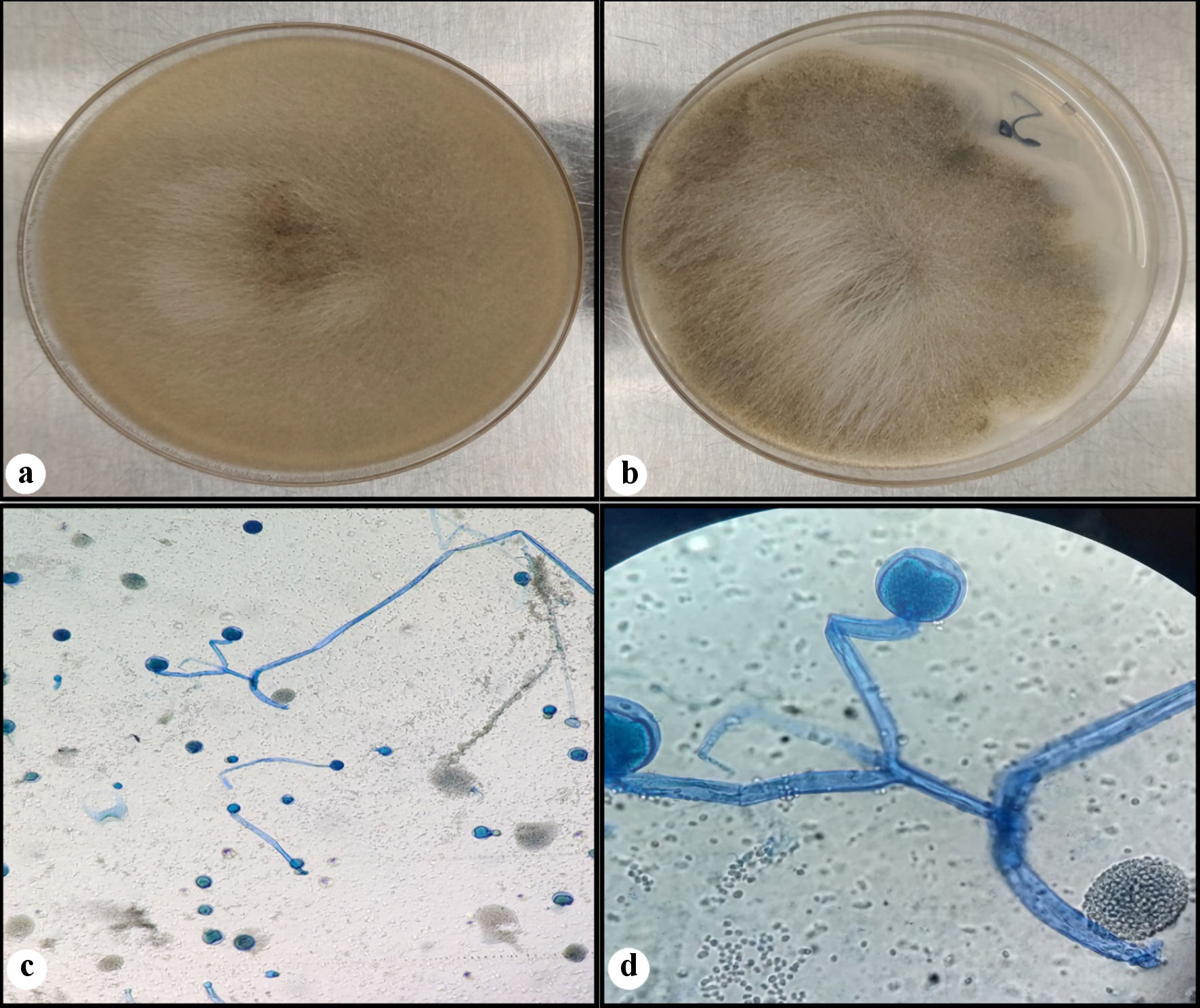
Figure 2. Fungal culture. Rapidly growing white fluffy colony that overfills agar plate on the Sabouraud dextrose agar (SDA) (a), and almost completely filling the potato dextrose agar (PDA) (b). A lactophenol cotton blue (LCB) preparation (c, d) showing wide hyphae, rare septations, branched sporangiophores, with round sporangia (sac-like structure). (d) Seen in the background are some spores of ruptured sporangium.