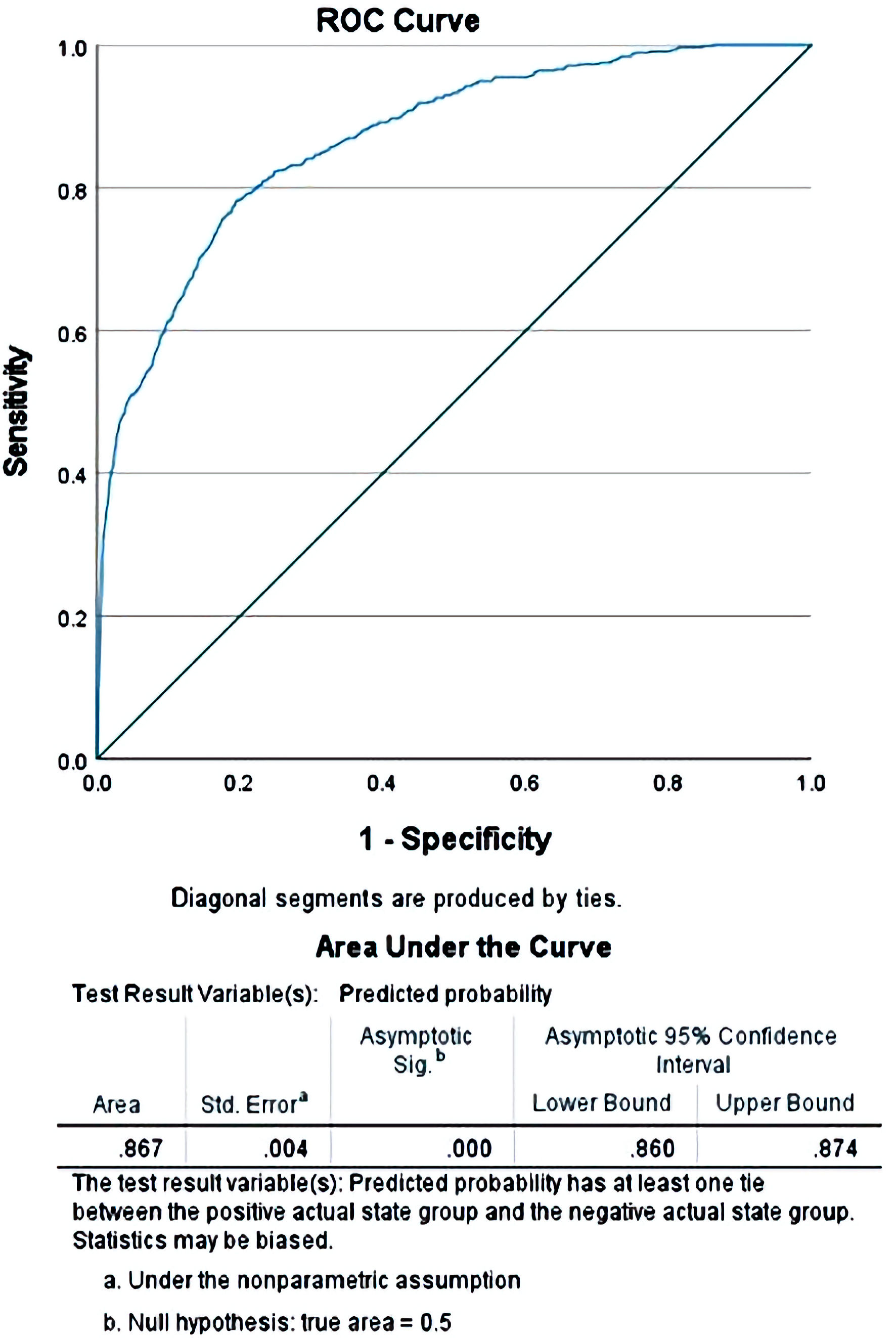
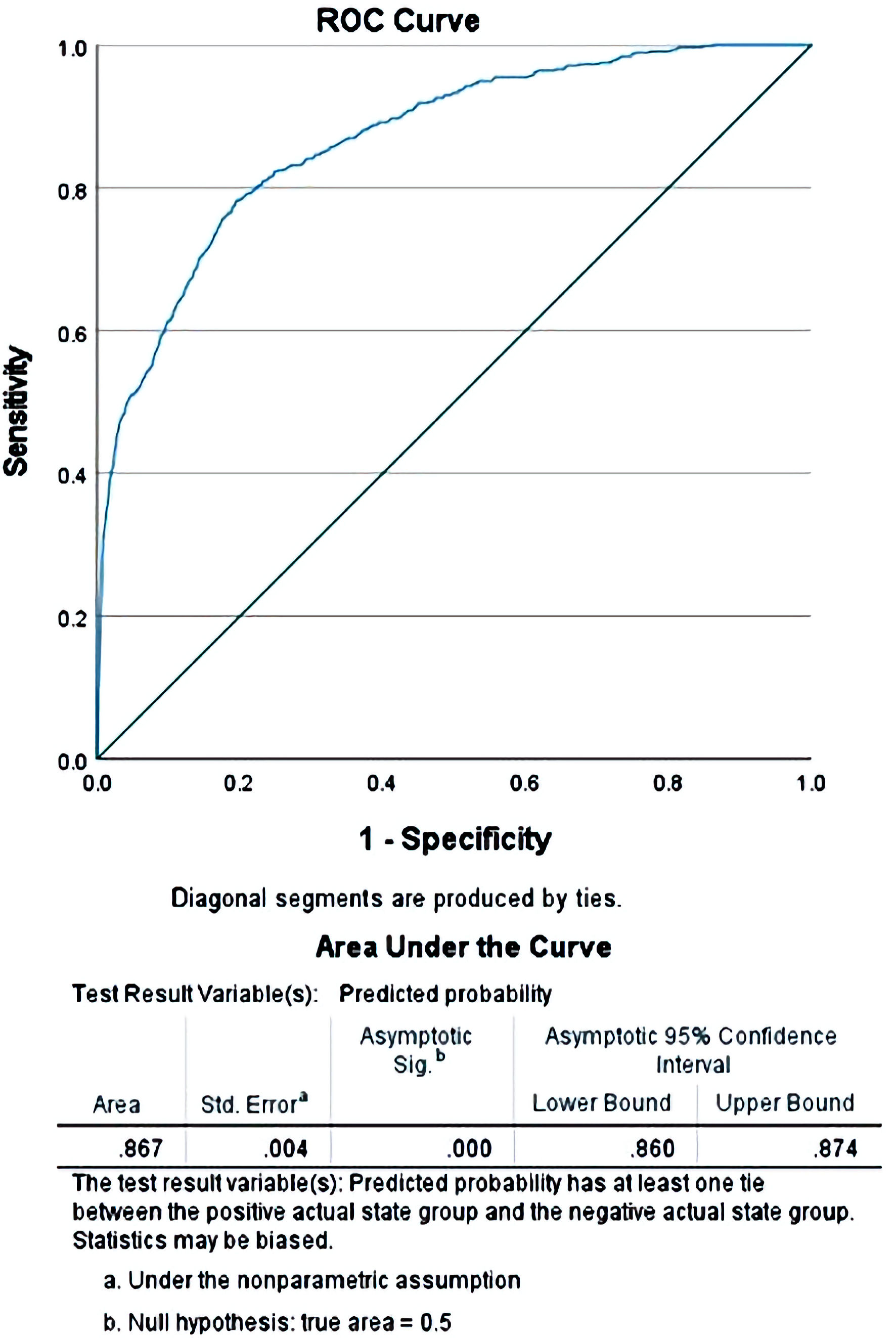
Figure 1. Receiver operating curve (ROC) comparing the predicted values of mortality obtained after the binary regression when compared with the observed values for the cases in the study.
| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 4, August 2022, pages 162-172
Early Colonoscopy in Hospitalized Patients With Acute Lower Gastrointestinal Bleeding: A Nationwide Analysis
Figure
Tables
| Diagnosis | Frequency (%b) | Frequency for colonoscopy patients (%b) |
|---|---|---|
| aAll numbers are weighted by NIS weight. bThe sum of all % values may add up to > 100 as some patients may have multiple diagnoses listed in their problem list. LGIB: lower gastrointestinal bleed; NIS: National (Nationwide) Inpatient Sample; ICD-10: International Classification of Disease 10th Edition. | ||
| Anorectal bleed | 119,330 (7.7%) | 23,940 (8.4%) |
| Diverticulosis | 271,095 (17.5%) | 122,720 (43.0%) |
| Diverticulitis | 44,430 (2.9%) | 7,835 (2.7%) |
| Angiodysplasia | 90,420 (5.8%) | 12,920 (4.5%) |
| Dieulafoy lesion | 5,585 (0.4%) | 1,190 (0.4%) |
| Melena | 896,325 (57.8%) | 112,870 (39.6%) |
| LGIB (primary diagnosis) with polyps, or benign neoplasm of large intestine (as secondary diagnosis) | 49,070 (3.2%) | 7,695 (2.7%) |
| LGIB (primary diagnosis) with malignant neoplasm of large intestine (as secondary diagnosis) | 5,190 (0.3%) | 635 (0.2%) |
| LGIB (primary diagnosis) with malignant neoplasm of anus (as secondary diagnosis) | 135 (0%) | 10 (0%) |
| LGIB (primary diagnosis) with malignant neoplasm of small intestine (as secondary diagnosis) | 295 (0%) | 15 (0%) |
| LGIB (primary diagnosis) with ischemia of intestine (as secondary diagnosis) | 10,965 (0.7%) | 2,365 (0.8%) |
| LGIB (primary diagnosis) with noninfectious colitis (as secondary diagnosis) | 11,705 (0.8%) | 1,535 (0.5%) |
| LGIB (primary diagnosis) with infectious colitis (as secondary diagnosis) | 1,305 (0.1%) | 75 (0%) |
| LGIB (primary diagnosis) with Crohn’s disease (as secondary diagnosis) | 13,560 (0.9%) | 1,065 (0.4%) |
| LGIB (primary diagnosis) with ulcerative colitis (as secondary diagnosis) | 48,515 (3.1%) | 2,410 (0.8%) |
| LGIB (primary diagnosis) with large intestinal fistula (as secondary diagnosis) | 1,015 (0.1%) | 350 (0.1%) |
| LGIB (primary diagnosis) with anal fissure (as secondary diagnosis) | 75 (0%) | 15 (0%) |
| Patients that received a colonoscopy | 285,165 (18.4%) | |
| Patients that received an early colonoscopy | 107,055 (6.9%) | |
| Characteristic | Early colonoscopy | Delayed colonoscopy | P value/total number |
|---|---|---|---|
| aNumbers weighted by NIS weight. The total numbers in each category may not necessarily add up to n = 285,165 as some of the values may not have been reported in the database, leading to those cases being excluded from these calculations. bMedian values would be a more accurate measure of central tendency as compared to mean for this data. NIS: National (Nationwide) Inpatient Sample; CCI: Charlson Comorbidity Index; SD: standard deviation. | |||
| Age, medianb | 73 | 73 | < 0.001 |
| Age, mean (SD) | 70.90 (14.45) | 70.59 (14.39) | < 0.001 |
| Age group, (in years) | < 0.001 | ||
| 18 - 35 (% within age group) | 2,790 (37.9%) | 4,580 (62.1%) | 7,370 (100%) |
| 36 - 50 | 7,650 (37.7%) | 12,625 (62.3%) | 20,275 |
| 51 - 65 | 21,815 (36.4%) | 38,130 (63.6%) | 59,945 |
| > 66 | 74,800 (37.9%) | 122,775 (62.1%) | 197,575 |
| Gender | < 0.001 | ||
| Male (% within gender group) | 56,835 (39.3%) | 87,735 (60.7%) | 144,570 (100%) |
| Female | 50,190 (35.7%) | 90,350 (64.3%) | 140,540 |
| Race | < 0.001 | ||
| White (% within race group) | 68,995 (38.1%) | 112,245 (61.9%) | 181,240 (100%) |
| Black | 19,610 (35%) | 36,475 (65%) | 24,725 |
| Hispanic | 9,245 (37.4%) | 15,480 (62.6%) | 24,725 |
| Asian/Pacific Islander | 3,130 (43.4%) | 4,075 (56.6%) | 7,205 |
| Native American | 560 (35.2%) | 1,030 (64.8%) | 1,590 |
| Other | 2,300 (37.9%) | 3,765 (62.1%) | 6,065 |
| Type of insurance | < 0.001 | ||
| Medicare (% within group) | 75,360 (37.2%) | 127,485 (62.8%) | 202,845 (100%) |
| Medicaid | 6,850 (31.8%) | 14,710 (68.2%) | 21,560 |
| Private | 19,845 (42%) | 27,450 (58%) | 47,295 |
| Self-pay | 2,545 (36.1%) | 4,510 (63.9%) | 7.055 |
| No charge | 270 (36.7%) | 465 (63.3%) | 735 |
| Other | 2,070 (38.7%) | 3,280 (61.3%) | 5,350 |
| Charlson Comorbidity Index grouping | < 0.001 | ||
| 0 (% within group) | 4,740 (43%) | 6,280 (57%) | 11,020 (100%) |
| 1 | 5,565 (41.9%) | 7,705 (58.1%) | 13,270 |
| 2 | 9,170 (44.1%) | 11,640 (55.9%) | 20,810 |
| ≥ 3 | 87,580 (36.5%) | 152,485 (63.5%) | 240,065 |
| CCI, medianb | 5 | 5 | < 0.001 |
| CCI, mean (SD) | 4.62 (2.37) | 5.12 (2.48) | < 0.001 |
| Hospital location/teaching status | < 0.001 | ||
| Rural (% within group) | 2,090 (39.7%) | 3,180 (60.3%) | 5,270 (100%) |
| Urban nonteaching | 7,350 (40.9%) | 10,600 (59.1%) | 17,950 |
| Urban teaching | 17,155 (37.6%) | 28,500 (62.4%) | 45,655 |
| Admission day of the week | < 0.001 | ||
| Weekday admission (% within group) | 84,940 (39.5%) | 130,165 (60.5%) | 215,105 (100%) |
| Weekend admission | 22,115 (31.6%) | 47,945 (68.4%) | 70,060 |
| Event/intervention | Early colonoscopy (n = 107,045) | Delayed colonoscopy (n = 178,105) | P value |
|---|---|---|---|
| aAlthough we reported the mean values, the median value would be a more accurate measurement of central tendency for this data set. LOS: length of stay; TOTCHG: total charges of hospitalization; SD: standard deviation. | |||
| Transfusion of any blood products | 34,535 (32.3%) | 66,185 (37.2%) | < 0.001 |
| Transfusion of red cell related products only | 33,645 (31.4%) | 64,905 (36.4%) | < 0.001 |
| Hypovolemia or shock | 7,660 (7.2%) | 11,990 (6.7%) | < 0.001 |
| Acute kidney injury | 15,925 (14.9%) | 41,140 (23.1%) | < 0.001 |
| Dialysis | 1,525 (1.4%) | 4,330 (2.4%) | < 0.001 |
| Acute respiratory failure | 1,420 (1.3%) | 3,835 (2.2%) | < 0.001 |
| Ventilator support (h) | < 0.001 | ||
| < 24 h | 480 (0.4%) | 970 (0.5%) | |
| 24 - 96 h | 825 (0.8%) | 1,995 (1.1%) | |
| > 96 h | 510 (0.5%) | 2,485 (1.4%) | |
| Endoscopic destruction of large intestine lesions | 620 (0.6%) | 1,040 (0.6%) | 0.871 |
| Outcomes | |||
| Death (% within colonoscopy group) | 1,005 (0.9%) | 2,530 (1.4%) | < 0.001 |
| Median length of stay (LOS) | 3 days | 5 days | < 0.001 |
| Median total charges (TOTCHG) | $32,037 | $44,092 | < 0.001 |
| Meana LOS (Standard deviation) | 3.99 days (4.64) | 7.10 days (8.40) | < 0.001 |
| Meana TOTCHG (SD) | $49,722 (71,486) | $77,048 (133,027) | < 0.001 |
| Covariate/predictor | Adjusted odds ratio | 95% confidence interval | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| aTransformation was performed on the value to make its distribution more normal, to have a more stable regression. LGIB: lower gastrointestinal bleed; IV: intravenous; AKI: acute kidney injury. | ||||
| Age (square-root transformed value)a | 0.991 | 0.963 | 1.020 | 0.533 |
| Gender (female) | 1.006 | 0.926 | 1.092 | 0.894 |
| Early colonoscopy | 0.902 | 0.827 | 0.985 | 0.022 |
| Race | < 0.001 | |||
| White | 0.789 | 0.627 | 0.992 | 0.043 |
| Black | 0.449 | 0.351 | 0.575 | < 0.001 |
| Hispanic | 0.741 | 0.570 | 0.962 | 0.024 |
| Asian/Pacific Islander | 0.693 | 0.492 | 0.976 | 0.036 |
| Native American | 1.445 | 0.939 | 2.222 | 0.094 |
| Type of insurance | < 0.001 | |||
| Medicare | 0.828 | 0.612 | 1.121 | 0.222 |
| Medicaid | 1.044 | 0.748 | 1.457 | 0.800 |
| Private | 0.743 | 0.539 | 1.023 | 0.069 |
| Self-pay | 1.271 | 0.853 | 1.895 | 0.238 |
| No charge | 0 | 0 | 0 | 0.991 |
| Charlson Comorbidity Index | 1.154 | 1.133 | 1.176 | < 0.001 |
| Hypovolemia/shock | 2.961 | 2.694 | 3.255 | < 0.001 |
| IV blood product transfusion | 1.147 | 1.057 | 1.244 | < 0.001 |
| AKI | 0.306 | 0.282 | 0.333 | < 0.001 |
| Dialysis | 3.584 | 3.041 | 4.225 | < 0.001 |
| Respiratory failure | 21.916 | 19.873 | 24.17 | < 0.001 |
| Endoscopic intervention | 0.486 | 0.257 | 0.919 | 0.026 |
| Covariate/predictor | Unstandardized coefficients after reverse transformationa | 95% confidence interval | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| aTransformation was performed on the value to make its distribution more normal and to have a more stable regression. The values in this table are reverse-transformed to make them more interpretable. bAge underwent square-root transformation making interpretation of numbers difficult in this case. For categorical variables, the +/- sign represents the direction of the effect, and the coefficient represents the percentage change attributed to the said covariate. For example, respiratory failure, if present, causes the LOS to increase by (1.671 - 1= 0.671) or 67.1%. LGIB: lower gastrointestinal bleed; IV: intravenous; AKI: acute kidney injury. | ||||
| Constant | 3.715 days | 3.508 | 3.926 | < 0.001 |
| Age (square-root transformed value)b | 1.052 | 1.049 | 1.054 | < 0.001 |
| Gender (female) | 1.028 | 1.023 | 1.033 | < 0.001 |
| Early colonoscopy | -1.44 | -1.448 | -1.435 | < 0.001 |
| Race | ||||
| White | 1.005 | -1.006 | 1.016 | 0.433 |
| Black | 1.045 | 1.033 | 1.057 | < 0.001 |
| Hispanic | -1.011 | -1.026 | 1 | 0.055 |
| Asian/Pacific Islander | -1.039 | -1.056 | -1.023 | < 0.001 |
| Native American | -1.035 | -1.062 | -1.007 | 0.016 |
| Type of insurance | ||||
| Medicare | 1.072 | 1.014 | 1.132 | 0.015 |
| Medicaid | 1.167 | 1.104 | 1.233 | < 0.001 |
| Private | 1.072 | 1.014 | 1.132 | 0.016 |
| Self-pay | 1.084 | 1.026 | 1.148 | 0.005 |
| No charge | 1.007 | -1.062 | 1.074 | 0.864 |
| Charlson Comorbidity Index | 1.045 | 1.042 | 1.045 | < 0.001 |
| Hypovolemia/shock | 1.256 | 1.245 | 1.265 | < 0.001 |
| IV blood product transfusion | 1.135 | 1.132 | 1.14 | < 0.001 |
| AKI | 1.239 | 1.233 | 1.247 | < 0.001 |
| Dialysis | 1.183 | 1.167 | 1.199 | < 0.001 |
| Respiratory failure | 1.671 | 1.644 | 1.698 | < 0.001 |
| Endoscopic intervention | 1.268 | 1.236 | 1.297 | < 0.001 |
| Weekend admission | -1.028 | -1.033 | -1.023 | < 0.001 |
| Covariate/predictor | Reverse-transformed values of unstandardized coefficientsa | 95% confidence interval | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| aTransformation was performed on the value to make its distribution more normal and to have a more stable regression. The values in this table are reverse-transformed to make them more interpretable. bAge underwent square-root transformation making interpretation of numbers difficult in this case. For categorical variables, the +/- sign represents the direction of the effect, and the coefficient represents the percentage change attributed to the said covariate. For example, respiratory failure, if present, causes the TOTCHG to increase by (2.466 - 1 = 1.466) or 146.6%. LGIB: lower gastrointestinal bleed; IV: intravenous; AKI: acute kidney injury. | ||||
| Constant | 16,982 | 15,631 | 18,450 | < 0.001 |
| Age (square-root transformed value)b | 1.052 | 1.050 | 1.054 | < 0.001 |
| Gender (female) | 1.002 | 0.998 | 1.009 | 0.357 |
| Early colonoscopy | -1.288 | -1.294 | -1.279 | < 0.001 |
| Race | ||||
| White | 1.153 | 1.135 | 1.172 | < 0.001 |
| Black | 1.175 | 1.156 | 1.197 | < 0.001 |
| Hispanic | 1.459 | 1.432 | 1.486 | < 0.001 |
| Asian/Pacific Islander | 1.426 | 1.393 | 1.459 | < 0.001 |
| Native American | 1.033 | 0.991 | 1.074 | 0.119 |
| Type of insurance | ||||
| Medicare | 1.153 | 1.067 | 1.250 | < 0.001 |
| Medicaid | 1.259 | 1.161 | 1.365 | < 0.001 |
| Private | 1.183 | 1.091 | 1.282 | < 0.001 |
| Self-pay | 1.194 | 1.102 | 1.297 | < 0.001 |
| No charge | 1.186 | 1.079 | 1.306 | < 0.001 |
| Charlson Comorbidity Index | 1.062 | 1.060 | 1.067 | < 0.001 |
| Hypovolemia/shock | 1.514 | 1.496 | 1.531 | < 0.001 |
| IV blood product transfusion | 1.186 | 1.18 | 1.194 | < 0.001 |
| AKI | 1.312 | 1.303 | 1.321 | < 0.001 |
| Dialysis | 1.253 | 1.230 | 1.279 | < 0.001 |
| Respiratory failure | 2.466 | 2.410 | 2.523 | < 0.001 |
| Endoscopic intervention | 1.250 | 1.205 | 1.294 | < 0.001 |
| Weekend admission | -1.019 | -1.026 | -1.011 | < 0.001 |