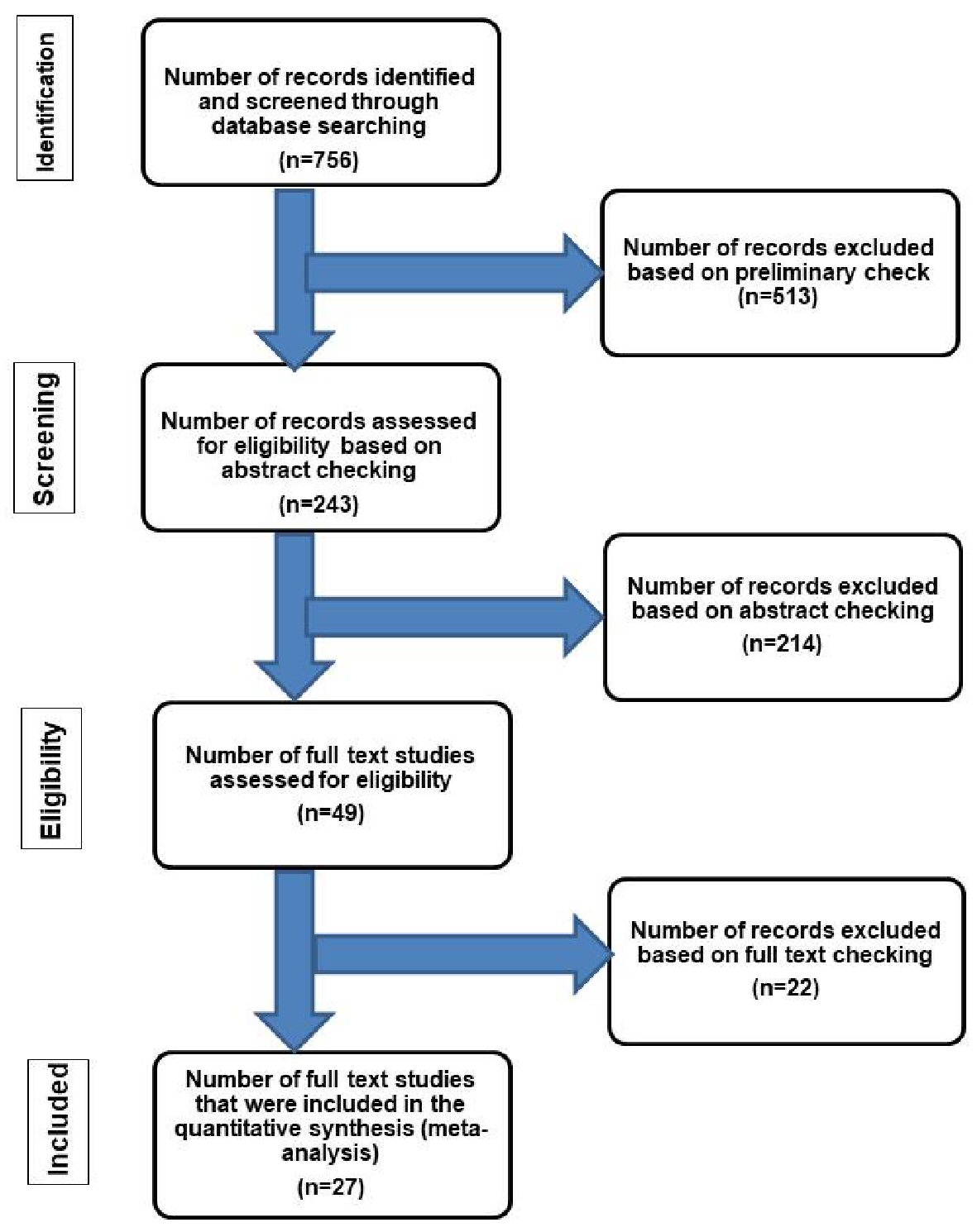
Figure 1. Flow chart of literature search and study selection for cases of localized intestinal amyloidosis. The inclusion criteria included patients who had amyloid deposition in the intestine without evidence of systemic involvement or an associated condition leading to secondary amyloidosis [42]. The exclusion criteria included patients with one or more of the followings: 1) Evidence of chronic diseases such as collagen vascular disease, that may have led to secondary amyloidosis [42]; 2) Additional organ involvement by amyloidosis; 3) Intestinal symptoms suggestive of amyloidosis but without confirmatory diagnostic tissue biopsy; 4) Plasma cell dyscrasia, myeloma, lymphoplasmacytic disorders or other B-cell malignancies such as Waldenstrom’s macroglobulinemia [5]; 5) Systemic AL type [43]; 6) Laboratory findings revealing positive detection of monoclonal light chains in serum and/or urine [15].